62 patients with 72 nodules at DCE-MRI were accrued. All patients underwent the 1st DCE-MRI at a median of 3.3 months (IQR: 3.1-4.1) after sRT, 33 patients (53.2%) presented a CR, 27 (43,5%) a PR, 2 (3.2%) no response. One patient, implanted with a cardiac device, did not undergo further MRI. Three more patients declined further testing after the 1st (N=2) or the 2nd (N=1) re-evaluation due to the COVID-19 pandemic. Twenty-eight patients underwent a 2nd DCE-MRI after a median of 6.8 months (IQR: 6.5-7.6) from sRT, 20 had a CR, 8 had a PR. After a median time of 10.7 months (IQR: 10.6-12.6), 6 patients were scanned for a 3nd DCE-MRI: 4 CR, 2 PR. The last patient reported a CR after 16.7 months.
The majority (94.3%, 95%CI: 88.0-100.0%) of lesions had completely disappeared by the 3rd re-evaluation or a median time of 10.7 months from the end of sRT (Figure).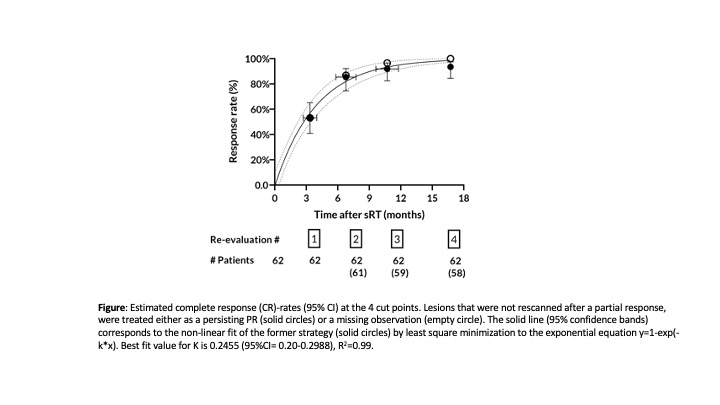
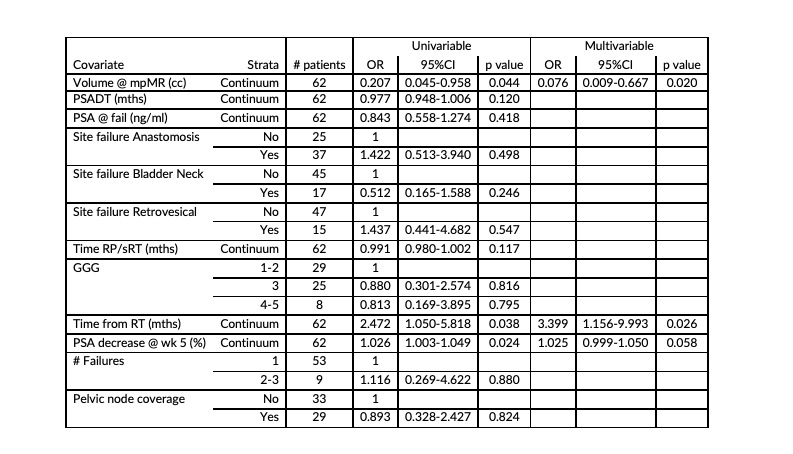
Independent predictors of CR at 1st re-evaluation on multivariable analysis were: the volume of the lesion at pre-sRT DCE-MRI (OR 0.076, 95%CI 0.009-0.667; p=0.02), the time of re-evaluation from treatment (OR 3.39, 95%CI 1.156-9.993; p=0.026) and the PSA percent decrease at the 5th week of sRT (OR 1.02, 95%CI 0.999-1.050; p= 0.058) (Table).
Receiver-operating characteristic curve (ROC) analysis identified the best cut-off on CR for baseline volume at 0.545 cc, AUC 0.683 (95%CI: 0.548-0.818, p=0.014). The probability of a CR for lesions larger than the cut-off identified at ROC analysis was only around 75% at 10.7 months.