The impact of a neuro-oncology RTT advanced practitioner in radiotherapy and proton beam therapy
PO-2292
Abstract
The impact of a neuro-oncology RTT advanced practitioner in radiotherapy and proton beam therapy
Authors: Karthica Santhagunanathan1, Amanda Webster1, Rita Simoes1
1University College London Hospital, Radiotherapy, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Brain, central nervous system (CNS) and intracranial tumours are the 9th most common cancers in the UK, accounting for 3% of all new cancer cases (2016-2018). To support patients through the pathway, a newly implemented neuro-oncology RTT advanced practitioner role was introduced in the radiotherapy (RT) and proton beam therapy (PBT) departments. The aim of this work is to assess the impact of the neuro-oncology RTT advanced practice (AP) role for patients with these tumour types and to ascertain improvements to the RT and PBT pathways.
Material and Methods
The evaluation was approved by the departmental governance group. An anonymous questionnaire was sent by post to 45 patients who were treated with radical RT or PBT for a CNS tumour between January – August 2022. The questionnaire (Table 1) was split into three sections to allow evaluation across the whole patient pathway; before, during and after treatment.
Table 1: Questionnaire:
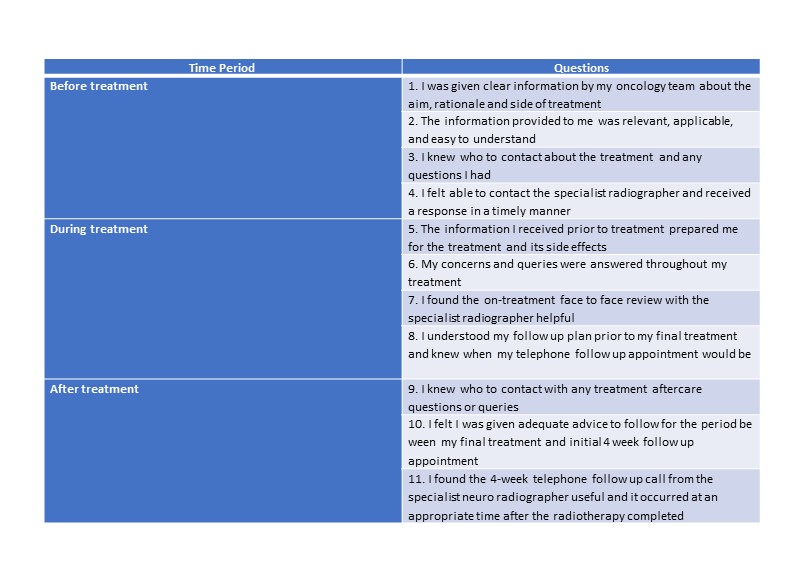
A Likert scale was used so that patients could score questions from 1-5, where 1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree and 5 = strongly agree. All data were anonymised and securely stored. Descriptive statistics were generated in Excel.
Results
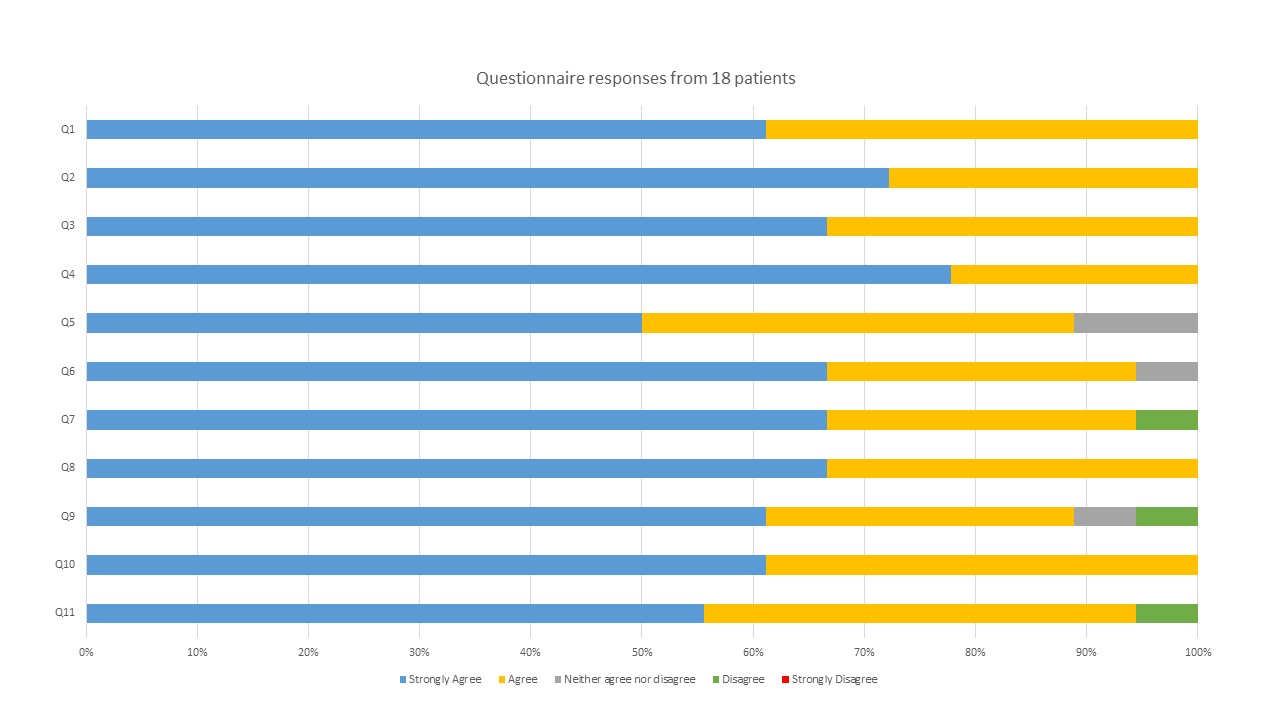
40% (n=18) of patients responded, and the data was analysed. Overall results were positive, showing between 50-78% of patients strongly agreed with the impact of the RTT AP. 94% (n=17) of patients strongly agreed or agreed to find the face-to-face review with the RTT AP helpful. One patient disagreed with knowing whom to contact with any aftercare questions, and one patient did not find the 4-week post-treatment telephone consultation helpful. 78% of patients gave additional comments, useful for further improvements, e.g., updating patient leaflets with contact details. Although given written information about treatment and its side effects and contact details for the RTT AP, 11% (n=2) still felt they were not prepared enough for the treatment.
Conclusion
This evaluation demonstrated the role of the RTT AP is valued to be a positive asset to patients in their pathway, at all-time points. There was evidence of simple improvements that could be made to the service. Patient leaflets could be discussed with patients to highlight contact details of whom to call with treatment queries. The RTT AP details could also be included in the patient leaflets as they may misplace the RTT AP business card given to them at time of consent. Improvements based on patients’ comments will be acted on, and further audited using the same questionnaire. Nonetheless, overall, this evaluation has demonstrated that patients valued the role of the RTT AP and highlights the unique support that RTTs can provide to patients during radiotherapy.