Digital play preparation for paediatric patients undergoing radiotherapy
Kim Robinson,
United Kingdom
PO-2291
Abstract
Digital play preparation for paediatric patients undergoing radiotherapy
1Royal Marsden Hospital, Radiotherapy, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Play therapy is used to help children through emotional times. For radiotherapy (RT) at the Royal Marsden Hospital (RMH) we use play to empower children, help them to understand what is happening and to encourage them to cooperate with RT procedures. Play helps the development of coping strategies and has been demonstrated to reduce the need for general anaesthesia (GA). Research from The University of Florida (Jacksonville, USA) supports this claim (Scott el al., 2016).
Following a review of available visual aids used to prepare patients for RT procedures at the RMH (Figure 1) we undertook a project to develop relevant and appropriate digital information packages to improve the preparation and support for children and their families.

Material and Methods
We created a multi-disciplinary team, including lead paediatric radiographers, play specialists, clinical oncologists and digital experts.
- Different methods of communication with children were explored and we discussed how to modernise the current visual aids
- A scoping exercise demonstrated children's preference for popular characters to use
- An artist from the charity 'Spread a Smile' was employed to make the immobilisation masks more child friendly
- We engaged a digital video team to create a video of the paediatric RT pathway at RMH
- A photographer was employed to take stills of the RT pathway for each character
Patient and public involvement (PPI) was engaged throughout.
Results
Tablet computers (iPads) were identified as the most appropriate medium and could be supported by the RMH IT system.
Immobilisation masks were made for each character and painted by the artist.
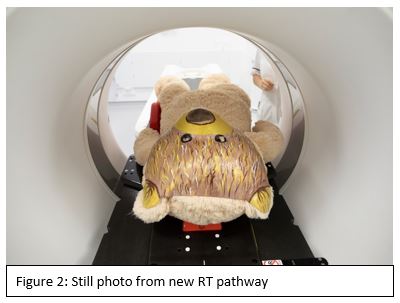
A still photograph was taken for each step of the RT pathway with different soft toys that were purchased for the project (Figure 2). This enabled each child to choose which character they would like to see as part of their preparation.
A script was written for the film crew to execute. Volunteers were sought from RMH and used in the video. A child actor and his father (also a professional actor) were cast in the film.
All aspects of the project were presented at a paediatric PPI event for feedback.
The project was shared RMH wide for information and feedback was welcomed.
The video is now available on the iPads and being used by all members of the MDT to prepare children. It can also be accessed by families at home to help with wider family engagement.
Conclusion
We have created appropriate and novel digital visual aids at RMH to prepare children and young people for RT.
Future work will review the impact of this project:
- Capture views, comments, 'likes' and downloads of the video from the RMH website
- Quantify if a reduction in GA is seen
- Survey patients and families to determine if they feel supported with the use of the new digital media
- Film other RT pathways to include the making of an immobilisation shell
- Expand the project using children and staff from more diverse backgrounds, prompted by initial PPI feedback