Identifying the priority areas for simulation in radiotherapy education: a Delphi study.
Sarah-Jane Ketterer,
United Kingdom
PO-2290
Abstract
Identifying the priority areas for simulation in radiotherapy education: a Delphi study.
Authors: Sarah-jane Ketterer1, Nicky Hutton1
1Society of Radiographers, Professional and Education, Liverpool, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Simulation based education has been identified as a key area for improving student experience and preparation for practice; offering an ideal opportunity to develop problem-solving skills in a safe environment, producing graduates who will be agile learners (1). Over the past decade there has been increased interest in the use of simulation as educators seek to optimise student experience and ensure placement opportunities are utilised effectively and efficiently (2,3). This study adopted a Delphi methodology to elicit consensus opinion on the priority areas for simulation within pre-registration therapeutic radiographer education.
Material and Methods
A multi-stage mixed method approach was undertaken, guided by a project steering group including representation from a range of stakeholders; Higher Education Institutions, clinical educators, patients, students, HCPC, AHP and simulation experts.
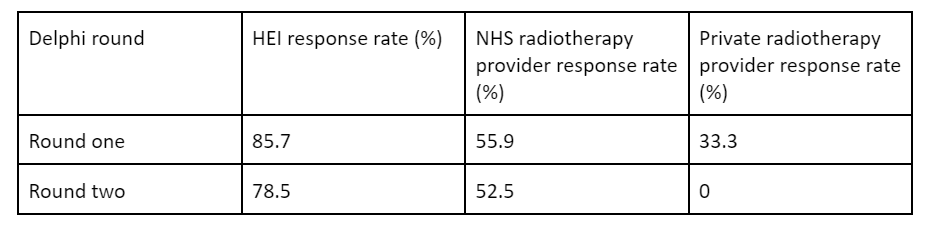
A Delphi study was conducted across UK HEIs n=14, UK NHS radiotherapy providers n=59 and UK private radiotherapy providers n=15 to gather consensus opinion on the priority areas for simulation within pre-registration education of therapeutic radiographers.
Round one sought to gain insight on all areas of the curriculum the panel felt could be delivered by simulation. Round two presented the themes from round one to participants and asked them to rank these based on their “importance” and “desirability” for delivery via simulation. Focus groups with student and patient representatives were utilised to supplement the Delphi data.
Results
Response rates to the Delphi survey were 57% for round one (n=50), and 48% (n=42) for round two. These were broken down by stakeholder demographic and detailed below.
All HEIs delivering pre-registration therapeutic radiographer training provide some form of simulation. Provision and access to facilities varied significantly, with challenges to wider implementation being largely resource focused.
Round one identified 104 areas of the curriculum that could be delivered via simulation. Thematic analysis was undertaken and results were grouped into 29 themes and returned to participants in round two.
Round two identified 15 themes that reached consensus; these were divided into four principal themes: communication, treatment and imaging scenarios, radiotherapy treatment planning and mandatory training, and were aligned to the HCPC Standards of Proficiency for Radiography (4).
Conclusion
The Delphi process provided a robust method for identifying priority areas of the radiotherapy curriculum to be delivered via simulation. Recommendations have been provided for areas where simulation could provide the most benefit within each year of training. The necessity for continued evaluation of simulation interventions to supplement the current evidence base, particularly in relation to achievement of learning outcomes, was highlighted. There is scope for significant future development and collaboration in terms of sharing of practice, and collaborative research initiatives.