Clinical implementation and evaluation of liver SBRT in breath-hold using nasal high flow therapy
PO-1388
Abstract
Clinical implementation and evaluation of liver SBRT in breath-hold using nasal high flow therapy
Authors: Colien Hazelaar1, Richard Canters1, Indra Lubken1, Kirsten Kremer1, Femke Vaassen1, Jeroen Buijsen1, Maaike Berbée1, Wouter van Elmpt1
1Department of Radiation Oncology (Maastro), GROW School for Oncology and Reproduction, Maastricht University Medical Centre+, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Breathing motion may result in large PTVs and poor CBCT image quality for patients treated with liver SBRT. To overcome this, we developed and implemented a markerless breath-hold liver SBRT technique using non-invasive nasal high flow therapy (NHFT) for breath-hold prolonging and surface-guided radiotherapy (SGRT) for breath-hold monitoring. In this study, we evaluate the first two years of clinical experience.
Material and Methods
Heated and humidified air was administered via a nasal cannula (40 L/min, 80% oxygen, 34°). Patients performed voluntary inspiration breath-holds supported by visual feedback within a 2 mm gating window. After a training session, 4 or 5 contrast-enhanced breath-hold CT scans were acquired to enable delineation of an ITV to account for inter- and intra-breath-hold variations. Patients were treated in 3–8 fractions using VMAT with 6 or 10 MV FFF beams using SGRT-controlled beam-hold. Patient setup was performed using SGRT and 4-DoF CBCT-CT matching based on the liver. After treatment, a CBCT scan was acquired for evaluation purposes.
Results
Between June 2020–June 2022, 17 liver SBRT patients started with the training session: 10 completed treatment in breath-hold, 5 continued in free-breathing (reasons: inability to understand procedure or position the arm above the head for a longer time and unreproducible or unstable breath-holds), 2 were not treated due to an increase in metastases. The average maximum breath-hold duration during treatment ranged per patient from 47–108 s. CBCT imaging took 60 seconds and half of all 100 scans were acquired during a single breath-hold. All patients could hold their breath for at least 60 seconds during one or more treatment fractions. For the 49 treatment fractions, the average number of breath-holds required for treatment was 6.6±4.1 (range: 2–19). The average time from CBCT before treatment to CBCT after treatment was 19±11 minutes (range: 9–51 min).
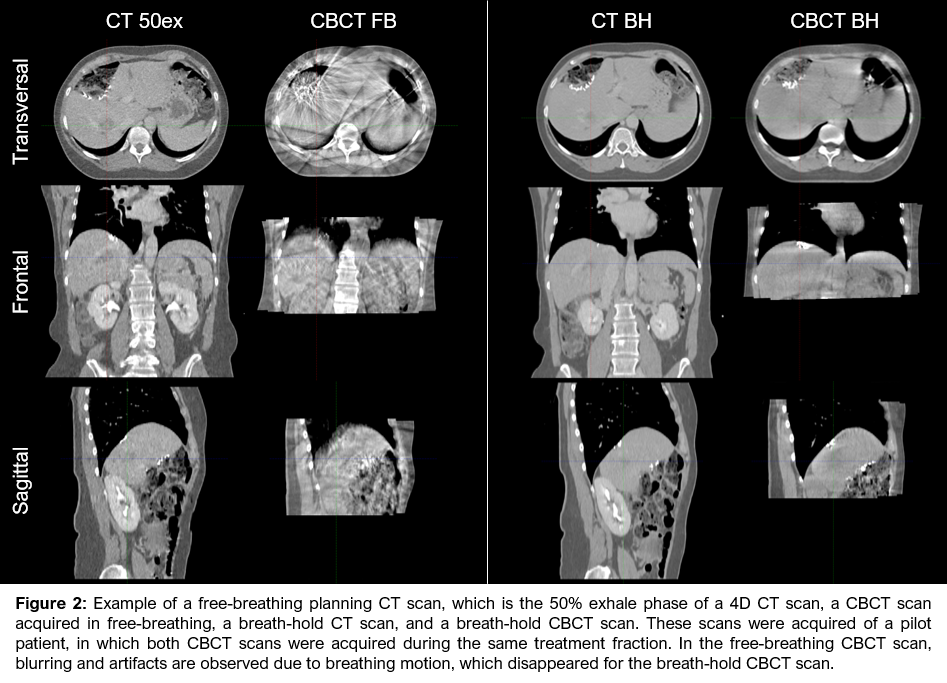
The difference in centroid position of the GTVs on the multiple planning CT scans was on average 3±3 mm for all directions (range: 0–10 mm). However, this difference was caused by a combination of breath-hold and delineation variations (volume differences ranged from 0.5–14.4 cm³). For all patients with a GTV difference >4 cm³, tumor visibility decreased over time due to the washout of contrast, resulting in smaller volumes on subsequent CT scans. The ITV was on average 6.3 cm³/28% larger (range: 1.1–23.9 cm³/5–72%) than the largest GTV. The 3D displacement vector for the 43 CBCT scans acquired after treatment was on average 5.0 mm (range: 0.7–12.9 mm; Figure 1) and for all but 2 scans less than our 1 cm PTV margin.
Conclusion
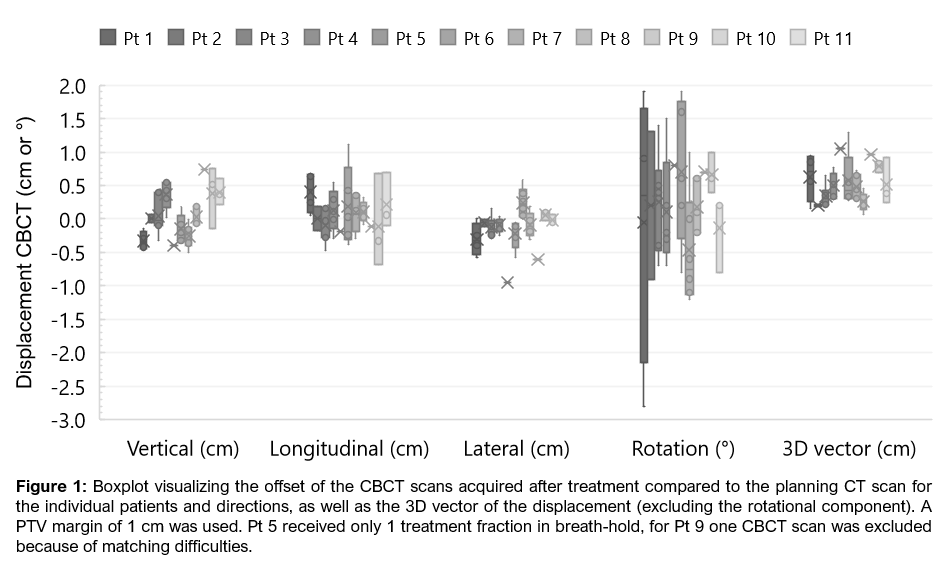
Liver SBRT in breath-hold using SGRT and prolonged breath-holds by NHFT is feasible for the majority of patients. Breath-holding resulted in high-quality CBCT imaging (Figure 2) that showed breath-hold variations smaller than the PTV margin. However, to further decrease the PTV, internal anatomy-based inter- and intra-breath-hold monitoring is desired.