Automated elective lymph level segmentation for head and neck cancer radiotherapy treatment planning
Victor Strijbis,
Switzerland
PO-1884
Abstract
Automated elective lymph level segmentation for head and neck cancer radiotherapy treatment planning
Authors: Victor Strijbis1, Max Dahele1, Oliver Gurney-Champion2, Berend Slotman1, Wilko Verbakel1
1Amsterdam UMC, Radiation Oncology, Amsterdam, The Netherlands; 2Amsterdam UMC, Radiology and Nuclear Medicine, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Head-and-neck cancer (HNC) radiation treatment (RT) planning requires
contouring of elective lymph nodes in the neck, however lymph levels that need
inclusion depend on clinical parameters. Therefore, a general, automated
segmentation approach for total elective lymph node volume cannot be used for
all locally advanced HNC. Deep learning (DL) has recently provided popular
means of automated segmentation. While DL for segmentation of combined elective
lymph node levels has been reported, we have evaluated and compared several DL
approaches for automated segmentation of individual levels.
Material and Methods
Bilateral lymph levels L1-L5 were manually contoured on computed tomography (CT) scans from 60 recent HNC patients. We trained and investigated
different model arrangements of a 3D patch-based U-Net and a multi-view
convolutional neural network (MV-CNN), which incorporates 2-dimensional views
of each orthogonal plane at multi-scale levels to classify the voxel where the
planes cross. Models were used either in a one-shot manner, to segment all
lymph levels directly, or in a sequential manner, where the total lymph node
volume is first segmented, followed by the MV-CNN to map foreground voxels to individual levels. Spatial performances from 5-fold cross-validation models
were evaluated using dice similarity coefficient (DSC) between model and manual
segmentations.
Results
The U-Net-MV-CNN sequential model outperformed other model arrangements,
with mean[median]± standard deviation DSC scores of 86[86]±3.1% for the total lymph node volume and 80[83]±15%, 84[85]±5.2%, 80[82]±7.6%, 75[79]±13%, 71[75]±14% for each level L1-L5 individually. Typical
example segmentations made with this model arrangement can be seen in Figure 1.
The one-shot solution by MV-CNN yielded median DSC scores of 74[77]±9.3%, 78[79]±5.5%, 70[75]±9.6%, 64[69]±15% and 68[70]±12% for individual lymph levels.
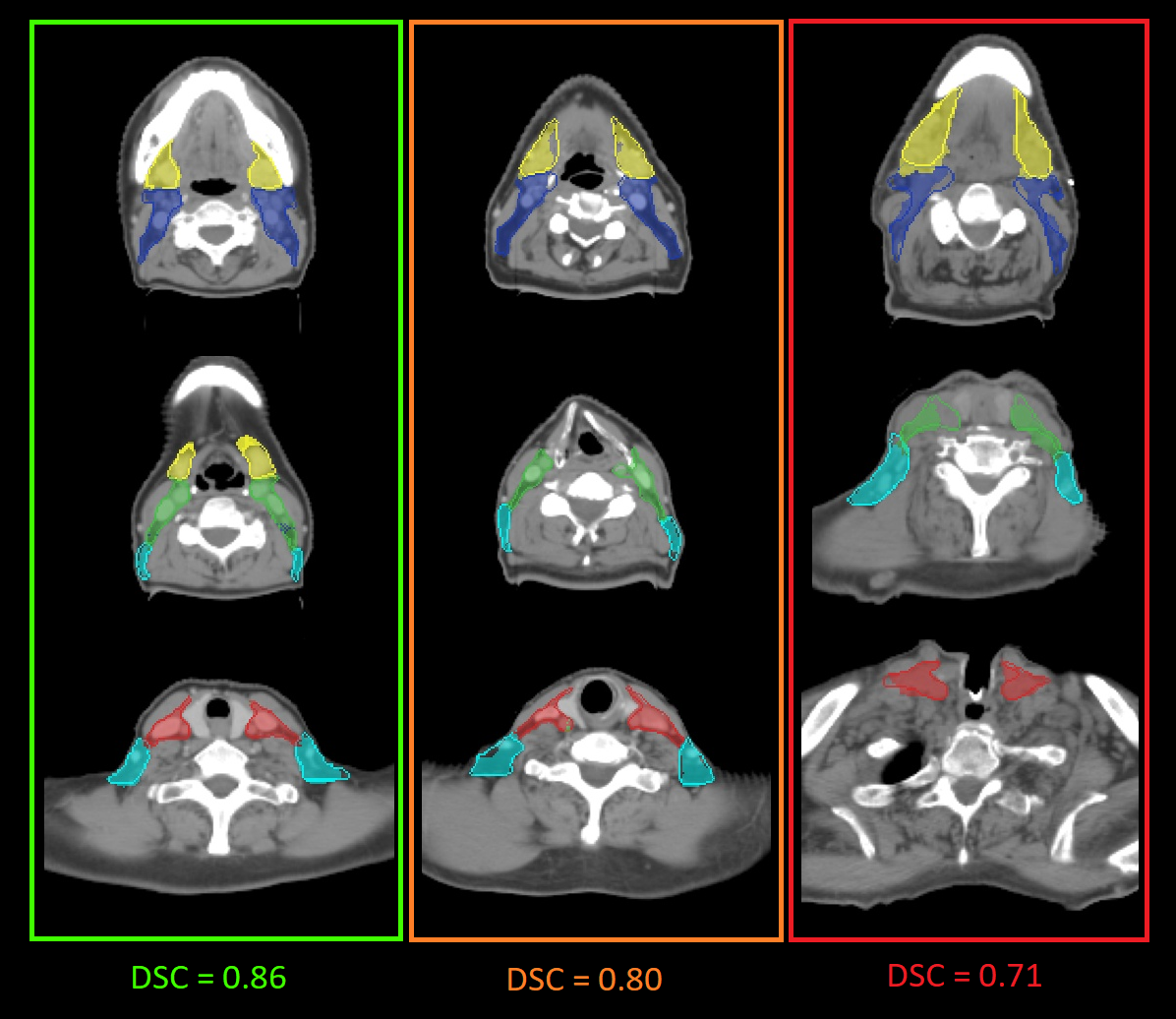
Figure 1 Example segmentations with good, average and poor typical cases are depicted in the green, orange and red
boxes, respectively. Reported DSC’s result from averaging over 5 contours. Lymph
levels L1-L5 are displayed in yellow, blue, green, red and cyan, respectively.
The opaque voxels show the 3D-border of the manual contour. Abbreviations: DSC: dice
similarity coefficient
Conclusion
We investigated several automated approaches for auto-contouring lymph
levels L1-L5. Although substantial variation between cases persists, requiring further investigation to minimize the need for manual checking for fully automated workflows, to the best of our knowledge, this is the first study to
demonstrate that accurate (median DSC>0.8) contours of individual lymph
levels can be obtained using DL methods.