Axillary lymph node boost: simultaneously integrated on CBCT-Linac or sequential on MR-Linac?
Roel Bouwmans,
The Netherlands
PO-1881
Abstract
Axillary lymph node boost: simultaneously integrated on CBCT-Linac or sequential on MR-Linac?
Authors: Roel Bouwmans1, Maureen Groot Koerkamp1, Femke Van der Leij1, Gijsbert Bol1, Alexis Kotte1, Anette Houweling1
1UMC Utrecht, Radiotherapy, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
In our clinical practice, breast cancer
patients requiring a boost dose to positive axillary lymph nodes, are treated
with a simultaneously integrated boost (SIB) technique. Position verification with
CBCT is performed for the full axillary lymph node region, the PTV margins
cover anatomical variation between boost volume and lymph node regions. With a
sequential boost given on a magnetic resonance (MR)-Linac, the plan can be
re-optimized to optimally target the boost volume thus allowing smaller
treatment margins. The SIB technique is less suited for the MR-Linac, mainly
due to the large extend of the treated volume compared to the limited field
size on the MR-Linac.
Our aim was to investigate the potential
benefit of an MR-Linac (Unity, Elekta) for irradiation of axillary lymph nodes
with a sequential boost, relative to our regular SIB technique. The hypothesis
is that we achieve a lower organ at risk (OAR) dose using the sequential
technique, while the same target dose is achieved.
Material and Methods
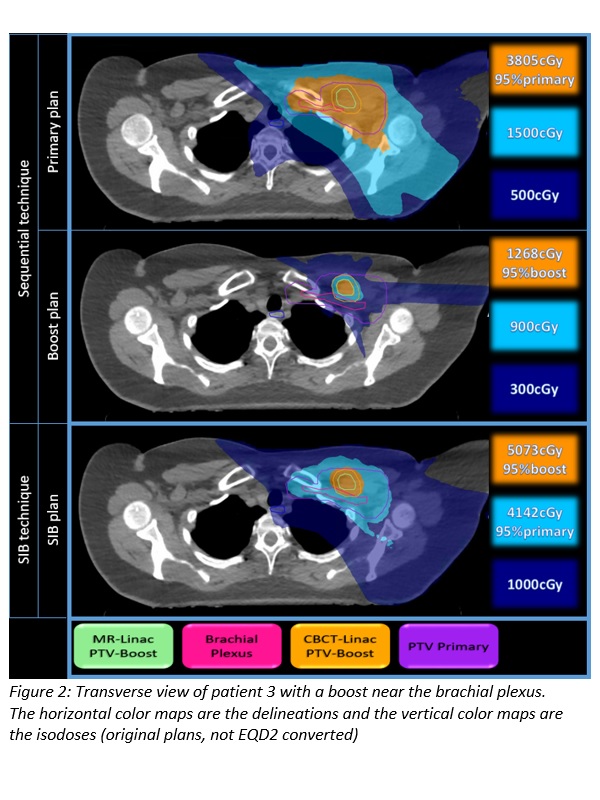
We performed a plan comparison (Monaco,
Elekta) for 7 breast cancer patients who received SIB treatment to axillary
lymph node(s), with or without local breast/chest wall radiotherapy. We compared
2 techniques per patient: a SIB technique for the CBCT-Linac (20x2.67Gy using
VMAT), and a sequential technique consisting of a primary CBCT-Linac plan
(15x2.67Gy using VMAT) and an MR-Linac boost plan (5x2.67Gy with IMRT). To investigate the maximal achievable benefit of the sequential
technique, a PTV boost margin of 0mm for the MR-Linac plan was used instead of
the 5mm margin used for the SIB technique. Both techniques
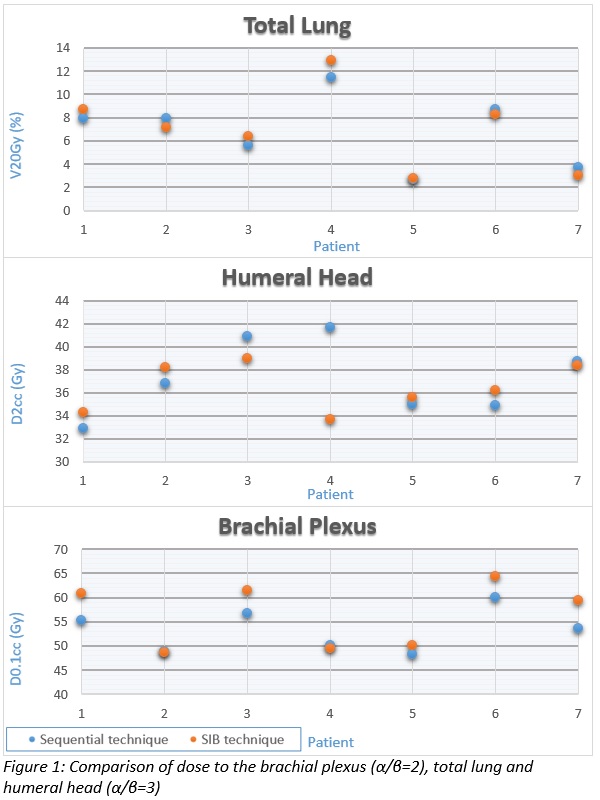
were converted to EQD2 for DVH analysis with α/β=2 for the brachial
plexus (D0.1cc) and α/β=3 for the total lung (V20Gy and Dmean) and humeral head
(D2% and Dmean).
Results
All plans were clinically acceptable
according to the institutional guidelines. The average DVH parameters were (SIB
technique vs. sequential technique) V95% PTV-boost: 98.6% vs. 97.9%; V20Gy total
lung: 7% vs. 6.8%; Dmean total lung was similar for both techniques: 4.3Gy; D2%
humeral head: 36.5Gy vs. 37.2Gy; Dmean humeral head: 16.5Gy vs 17Gy; D0.1cc
brachial plexus: 56.3Gy vs 53.3Gy.
For 4 of the 7 patients there was a
larger difference in the D0.1cc of the brachial plexus (figure 1), because the
boost location was close to the brachial plexus (figure 2).
Conclusion
Even with a 0mm PTV margin, the overall
difference between both techniques is limited. For specific patients with an
OAR close to the lymph node boost, the MR-Linac based sequential boost was
beneficial over the SIB technique.