Trade-off in lung and heart dose and the impact on target robustness in VMAT of oesophageal cancer
Sabine Visser,
The Netherlands
PO-1879
Abstract
Trade-off in lung and heart dose and the impact on target robustness in VMAT of oesophageal cancer
Authors: Sabine Visser1, Martje Schol1, Petra Klinker1, Margriet Dieters1, Veronique E. Mul1, Johannes A. Langendijk1, Erik W. Korevaar1, Stefan Both1, Christina T. Muijs1
1UMCG, Radiotherapy, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
In the
radiotherapy treatment of oesophageal cancer (EC), the lungs and heart are in
close proximity of the target volume. Reducing lung dose was historically the
primary aim in treatment planning. However, due to increased awareness of the
risk of cardiac complications after radiotherapy, the optimisation process
nowadays is more focused on reducing heart dose. The result is an increased
lateral dose contribution which may lead to less robust treatment plans. In
this study, we explored the trade-off between heart and lung dose, and
corresponding target robustness.
Material and Methods
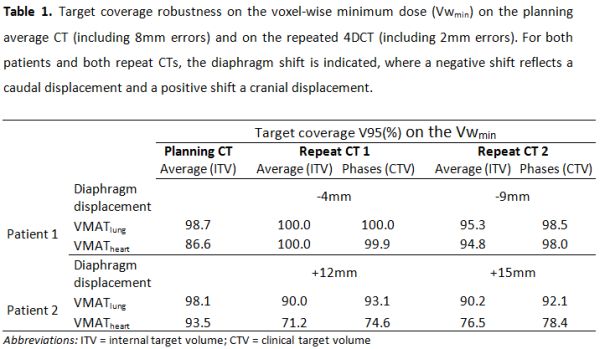
Two EC
patients were selected for this study, who presented diaphragm displacements
during treatment (Table 1). Target volumes were delineated on the phases and
the average of the planning 4DCT, and of two repeated 4DCTs. For each patient,
two volumetric modulated arc therapy (VMAT) plans were created to cover the
planning target volume; one with the aim to reduce mean lung dose (MLD) as much
as possible (VMATlung) and one with the aim to reduce mean heart
dose (MHD) as much as possible (VMATheart). Both plans had to obey
priority 1 and 2 constraints as defined in our clinic (MHD <26 Gy; MLD
<16 Gy). First, we investigated the presumed static dose cloud of the plans by
shifting the isocenter 8mm in all directions on the planning image. The
resulting 14 dose scenarios were summarized in a voxel-wise minimum dose
distribution to evaluate target coverage. Additionally, the plan was robustly
evaluated (including 2mm shifts to account for residual uncertainties) on the
repeated 4DCTs, using the average and using accumulative dose of all the phases.
Results
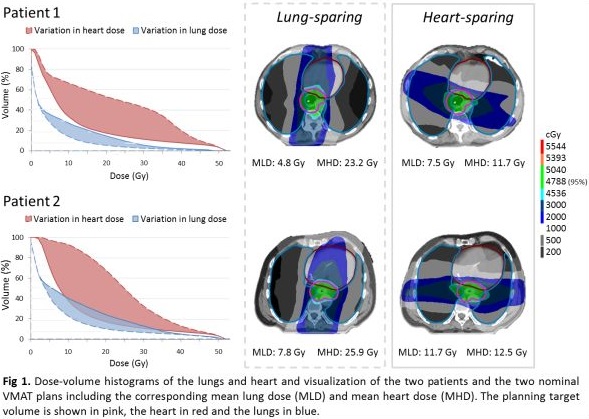
For
both patients, the optimisation window of heart dose was substantially larger
than that of lung dose comparing VMATlung and VMATheart
(Figure 1). The average MHD reduction was 12.5 Gy comparing VMATheart
to VMATlung, while on average the MLD increased by 3.3 Gy. Robust
evaluation at baseline suggested reduced target robustness for the VMATheart
plans, compared to the VMATlung plans (Table 1). Variations in the
diaphragm position resulted in reduced target coverage on the repeated CT. This
was especially true for the VMATheart plans if the diaphragm moved cranially
as observed for patient 2. On the opposite, the diaphragm moved caudally for
patient 1 and hotspots were observed in the heart region for VMATheart.
For both patients, the changes in diaphragm position were consistent along the
treatment. When all phases were considered, target coverage slightly improved,
as the dose averaged out. However, target underdosage was still present for
patient 2 (V95: 74-79%).
Conclusion
In
VMAT radiotherapy for EC, the heart can be spared without a substantial
increase in MLD. However, this results in increased risk of underdosage if the
diaphragm shifts in cranial direction or cardiac hotspots if it shifts in
caudal direction. Robustness evaluation of the treatment plan seems to indicate
these risks already at baseline.