Initial experience delivering stereotactic radiotherapy to a gluteal metastasis on a 1.5T MR Linac
Phil Fendall Amaro,
United Kingdom
PO-1877
Abstract
Initial experience delivering stereotactic radiotherapy to a gluteal metastasis on a 1.5T MR Linac
Authors: Phil Teles Amaro1, Lisa McDaid1, Lucy Davies1, Lee Whiteside1, Abigael Clough1, Corinne Faivre-Finn2,3, Jacqui Parker1, Rachael Bailey1, Rebecca Benson1, Claire Nelder1, Eleanor Pitt1, Cynthia Eccles1,4, Cathryn Crockett2, Ahmed Salem2, Ananya Choudhury2,5
1The Christie NHS Foundation Trust, Radiotherapy, Manchester, United Kingdom; 2The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom; 3University of Manchester, Radiation Oncology, Manchester, United Kingdom; 4University of Manchester, Medicine and health, Manchester, United Kingdom; 5University of Manchester, Cancer Sciences, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
This work reports on our initial experience delivering
stereotactic ablative radiotherapy (SABR) to a gluteal metastasis on a 1.5T Elekta
Unity MR Linac (MRL) (Elekta AB. Stockholm, Sweden).
Material and Methods
A patient with non-small cell lung cancer (NSCLC) was found
to have an 8mm right-sided gluteal oligometastasis on staging FDG PET-CT (stage
IVa, oligometastatic disease). Discussion at local SABR multi-disciplinary team
(MDT) highlighted challenges in localising the sub-centimetre gluteal
metastasis on cone-beam CT (CBCT) imaging, therefore a referral was made for
treatment on the MRL within the ethically approved, imaging study PRIMER
(Clinicaltrials.gov NCT02973828).
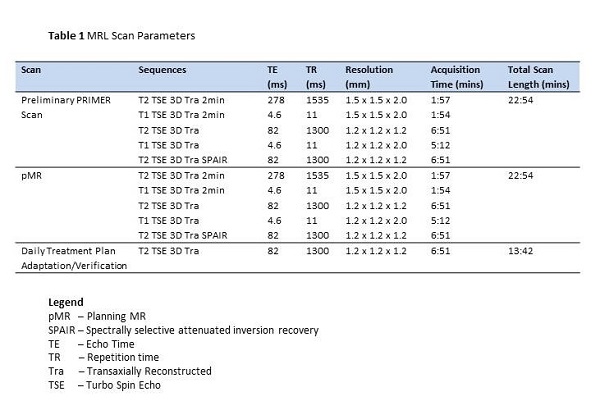
A preliminary MR scan was performed to ensure the lesion was
identifiable. Vendor approved MR sequences (Table 1) were used to determine lesion
conspicuity as, ultimately, only these sequences are sanctioned for clinical
use on the Unity MRL. A further spectrally selective attenuated inversion
recovery (SPAIR) sequence was performed to suppress fat signal and provide
further confidence in disease visibility. The patient then underwent CT and MR
planning scans (pCT and pMR respectively), positioned supine with arms on
thorax and pelvis immobilised with knee and foot step. pCT was performed for
the provision of electron density data to inform treatment planning.
pCT and pMR image sets were imported into the Monaco treatment
planning system (v 5.40.01, Elekta AB. Stockholm, Sweden) for target volume and
organ at risk (OAR) delineation and a prescription of 30Gy in 3 fractions was
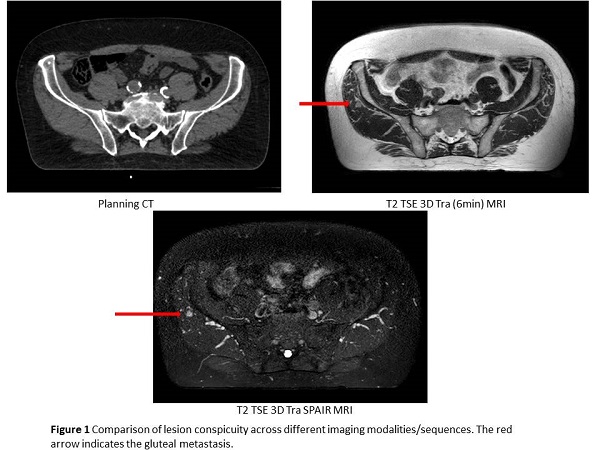
planned. The T2 SPAIR sequence was co-registered with the 6 minute T2 3D Tra sequence
to further aid target delineation.
Results
Delivery of SABR (30Gy in 3 fractions over 6 days) to
a gluteal oligometastasis was successfully completed on the Unity MRL following
the Adapt to Position (ATP) workflow. Target visualisation on pMR was superior
to pCT, in which the 8mm lesion was barely visible (Figure 1). Consensus review
showed that the 6 minute T2 3D Tra sequence provided superior confidence in
target visibility and was therefore used for planning and daily plan
adaptation/verification. Median treatment time was 52:08 (range 49:19 - 57:16).
The patient did not report any adverse effects.
Conclusion
We have successfully completed SABR delivery to a sub-centimetre
oligometastasis within the right gluteus medius muscle on the Elekta Unity MRL
following the ATP workflow, a first at our institution. This would not
have been possible on a conventional linac due to the poor soft-tissue contrast
associated with CT and CBCT imaging. Workflows have been established that will
facilitate a future MR guided, soft tissue tumour service.