Infleunces of Interfractional changes of rectum/bladder on vagina motion in endometrium radiotherapy
PO-1841
Abstract
Infleunces of Interfractional changes of rectum/bladder on vagina motion in endometrium radiotherapy
Authors: Yatman Tsang1, Amirah Abduallah2, Adele Stewart-Lord3, Daniel Megias1, Hannah Tharmalingam4, Peter Hoskin4
1Mount Vernon Cancer Centre, Radiotherapy, Northwood, United Kingdom; 2Mount Vernon Cancer Centre, Radiotherapy , Northwood, United Kingdom; 3London Southbank University , Institute of Health and Social Care, London, United Kingdom; 4Mount Vernon Cancer Centre, Clinical Oncology, Northwood, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate the influence of interfractional position and volumetric changes of the bladder and rectum on vagina displacements during postoperative external beam radiotherapy (EBRT) of endometrial cancer.
Material and Methods
In a single centre retrospective cohort study, measurements of interfractional displacements and volumetric changes of bladder, rectum and vagina were carried out for 28 patients that underwent EBRT for endometria tumours. Measurements were carried out on initial planning computer tomography (CT) scans and on daily cone beam computer tomography (CBCT) scans. Rectum displacements were determined by measuring anterior-posterior (AP) rectal diameters at S5 vertebrae and 4 cm inferior to S5 level. Bladder volumetric changes were determined via measure of AP bladder diameter and superior-inferior (SI) bladder diameter. Vaginal displacements were determined by measure of difference in distances from the pubic symphysis and from the S5 vertebrae at planning CT scans and daily CBCT scans. Wilcoxon signed-rank test was used to analyse the significance in displacement of the rectum/bladder and vagina between planning CT scans and daily CBCT scans. Spearman’s rank-order correlation was then used to analyse significance of the association of changes in rectum and bladder with the displacement of the vagina from planning CT scans to daily CBCT scans.
Results
28 initial planning CT scans and 756 CBCT scans were analysed.
Significant interfractional changes in rectum position, bladder volume and vagina position were determined between planning CT scans and daily CBCT scans. No statistically significant correlations were found between interfractional changes of bladder and vaginal displacements.
Weak relations were found
(i) between increase in rectal AP diameter and increase in vaginal displacement from S5 (rs=0.14 p value<0.0.1)
(ii) between increase in rectal AP diameter and increase in vaginal displacement from 4cm inferior to S5 (rs=0.22 p value<0.05)
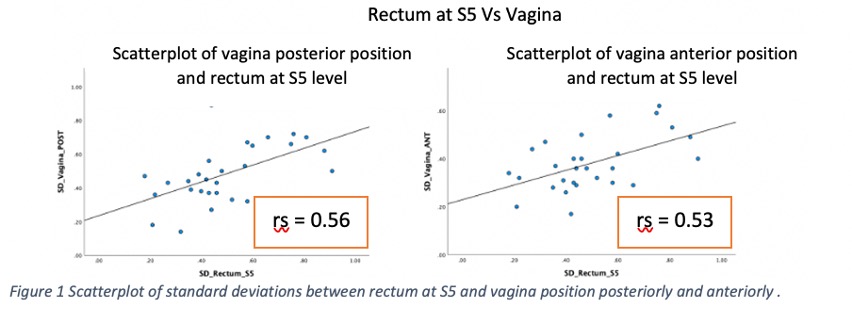
Greater interfractional changes in vaginal positions were found in patients who had larger interfractional variations in rectal volumes (Figure 1).
Conclusion
The findings of this study highlight that better strategies to ensure reproducible rectal volume and position in postoperative endometrium EBRT are required. Patient specific relation between interfractional changes of the rectum with vaginal displacements reinforce the importance of individualised internal target volume (ITV) margins and online daily image guided radiation therapy (IGRT).