A dosimetric study of dose algorithm impact and number of VMAT arcs in single fraction lung SBRT.
Wei Yang Calvin Koh,
Singapore
PO-1741
Abstract
A dosimetric study of dose algorithm impact and number of VMAT arcs in single fraction lung SBRT.
Authors: Wei Yang Calvin Koh1, Hong Qi Tan1, Yan Yee Ng1, Khong Wei Ang1, Kah Seng Lew1, Yen Hwa Lin1, Ghee Ann Clifford Chua1, Haw Hwong Jerome Yap1, Jun Hao Phua1, Yun Ming Wong1, Sung Yong Park1, James Cheow Lei Lee1
1National Cancer Centre Singapore, Radiation Oncology, Singapore, Singapore
Show Affiliations
Hide Affiliations
Purpose or Objective
TROG 13.01 SAFRON II have shown similar 1-year toxicity, OS, PFS and local control between single and multi fractions
Lung SBRT. While preparing the planning protocol for single
fraction Lung SBRT, dosimetric measurements for different dose
calculation algorithms and a different number of VMAT arcs were performed to ensure plan
deliverability and agreement between planning and delivered dose (28Gy/1 fraction).
Material and Methods
5 VMAT plans (AXB-6FFF-3A, AXB-10FFF-3A, AAA-10FFF-3A, AAA-10FFF-4A and AAA-10FFF-6A) were output by an experienced dosimetrist on 5 retrospective patients. 3A, 4A and 6A denote the number of radiation beam arcs and AXB or AAA refers to the dose algorithm used for optimizing
the plan. 1mm and 2mm calculation grid size and
dose to medium were used in dose reporting for AXB algorithm. PSQA
was performed using point-dose measurement (Static QUASARTM phantom with Cedarwood insert; both Pinpoint and Farmer Chamber from PTW were used) and PD. Global gamma passing rates at 1%/1mm, 2%/1mm, 1%/2mm and 2%/2mm
were reported for the PD QA. Lastly,
plan complexity comparisons were evaluated using modulation complexity score
(MCS) across all the
plans.
Results
The
results show that the 4A and 6A plans are less complex (P-value <
0.05) as compared to other plans and the respective MCS for each plan types for
all patients are as shown in Figure 1.
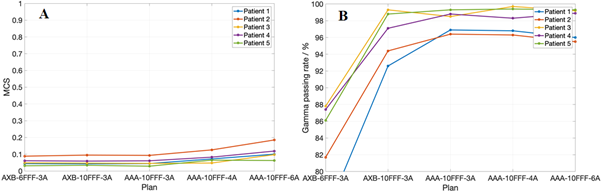
Figure
1(A) shows the MCS for all plan types across all patients and 1(B) shows the gamma
passing rate of 1mm/1% for all plan types across all patients.
The
point dose difference between measurement and plan calculated with
two different grid sizes using two different dose calculation algorithms are shown in Figure 2. All plans are evaluated to be less than 5% dose
discrepancy except AXB-6FFF-3A. This discrepancy result between 6FFF and 10FFF
is similar to that reported by Öllers
MC et al.[2]. The
least discrepancy occurs using the AXB dose calculation algorithm with a 1mm
calculation grid size. Subsequently, PSQA using PD was done and
the result follow a similar trend from point dose measurement. AXB-6FFF-3A
gives a lower gamma passing rate for all
criteria. Despite being less complex, 4 and 6 arcs plan does not result in a
statistically significant higher gamma passing rate. Lastly, the dose in OAR
and PTV were compared between the two different dose calculation algorithms.
The main differences occur in PTV D95 and D98 where using 6FFF beams gave less
than 1 Gy difference while 10FFF beams gave less than 3 Gy difference. The
difference in doses in the OARs are less than 0.5%.
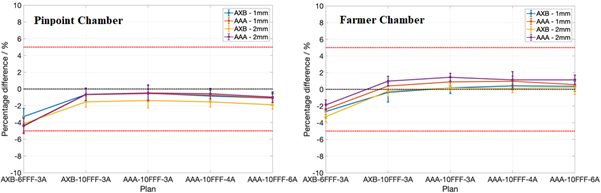
Figure
2 shows the percentage difference in point dose between treatment plans (AXB and AAA; 1mm and 2mm) and measurement (Pinpoint and Farmer).
Conclusion
This study shows that 10FFF beam is recommended for
hypo-fractionated treatment and similar dosimetric accuracy are obtained for 3,
4 and 6 arcs plan. The point dose measurement results also support the use of the
AXB dose calculation dose algorithm with a 1mm calculation grid size.