Evaluation of effect of two methods of dose prescription on dose distribution for lung tumors SBRT
PO-1735
Abstract
Evaluation of effect of two methods of dose prescription on dose distribution for lung tumors SBRT
Authors: Agnieszka Skrobala1,2, Justyna Kosmowska1, Marta Kruszyna-Mochalska3,2, Julian Malicki2
1Greater Poland Cancer Centre, Medical Physics Department, Poznan, Poland; 2Electroradiology Department, University of Medical Sciences, Poznan, Poland; 3Medical Physics Department, Greater Poland Cancer Centre, Poznan, Poland
Show Affiliations
Hide Affiliations
Purpose or Objective
The purpose of this study was the
evaluation the effect of two methods of dose prescription on dose distribution
for lung tumors treated by VMAT stereotactic radiotherapy in terms of plan
quality and analysis of accuracy in dose delivery.
Material and Methods
In total, 10 patients with left
lung tumors previously treated with VMAT stereotaxic radiotherapy were
examined. These patients were replaned using two methods of dose prescription.
The first, the administered dose of 50 Gy/5fr, was prescribed on 80% isodose
(80%plan), the second on 100% (100%plan) isodose covering PTV; normalization
was 98% of the prescribed dose received 98% of PTV. Both plans were three half-arcs VMAT with
6XFFF, TrueBeam (Varian, USA). Both plans (80%plan) and (100%plan) were
compared in terms of dose-volume metrics by RTOG conformity index (CI) and
gradient index (GI), and the constraints for the particular doses to OARs (reported
by Grimm et al. (Jacmp2011)) were evaluated. The number of monitor units (MU)
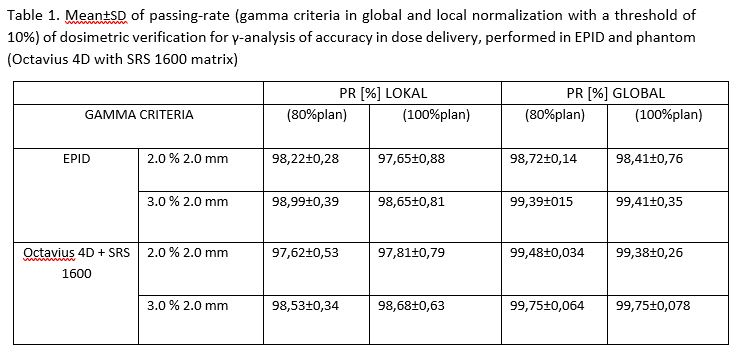
and were examined in terms of treatment time. Following gamma criteria in
global (G) and local (L) normalization with a threshold of 10%, were (G2%,2mm),
(G3%,2mm) and (L2%,2mm), (L3%,2mm) were used in the passing-rate (PR)
γ-analysis. Accuracy in dose delivery was performed in EPID and phantom
Octavius 4D with SRS 1600 matrix, PTW Freiburg. The accepted level for PR was
≥95%. The point dose was verified by dynamic phantom QUASAR (Modus Medical
Devices, Canada) Pinpoint (PTW Freiburg).
Results
Both 80% and 100% plans were
judged clinically acceptable, but more significant differences were noticed in
the plan quality parameters with the increasing volume of PTV. A significant
difference in both DmaxPTV and D2%PTV favoring (80%plan) plans was observed
(p<0.01). For (80%plan) and (100%plan) computed doses for OARs were not
equivalent, (80%plan) achieved lower values for Dmean thoracic wall 7.07 vs.
8.65Gy, Dmean lung 3.15 vs. 3.19Gy, left lung 5.61 vs. 5.77Gy and Dmax spinal
cord 10.05 vs. 16.84Gy. Finally, mean MU
for (80%plan) was 3644MU
and were reduced to 3305MU for (100%plan), values were significantly smaller for a
smaller volume of lesions. Acceptable results were obtained for adopted
criteria for both plans (80%plan) and (100%plan) and presented in table 1. The mean difference between measured and calculated
point doses were – 0,7Gy for (80%plan) and -0.48Gy for (100%plan) in the dynamic
phantom QUASAR.
Conclusion
Doses for lung tumors organs at
risk were comparable for both methods of dose prescription 80% and 100% treated
by VMAT stereotactic radiotherapy. However, in (80%plan) increased the dose for
PTV while reducing doses for surrounding tissues and organs at risk. CI and
other plan quality parameters were higher or slightly higher (80%plan). It was
shown that the overall treatment time for patients with (80%plan) was longer. The
dosimetric consistency between planned and delivered was satisfactory from (80%plan)
and (100%plan) independent of dosimetric methods.