Robust optimization for IMPT in head and neck cancer with coupled vs. uncoupled scenarios
Ulrik Vindelev Elstroem,
Denmark
PO-1727
Abstract
Robust optimization for IMPT in head and neck cancer with coupled vs. uncoupled scenarios
Authors: Ulrik Vindelev Elstroem1, Ole Noerrevang1, Kenneth Jensen1
1Aarhus University Hospital, Danish Center for Particle Therapy, Aarhus N, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
For intensity
modulated proton therapy (IMPT) planning, robust optimization (RO) and
evaluation is used to compensate for worst case uncertainties in dose deposition
due to translational changes in setup and stopping power (range). The two
uncertainties can be either coupled or uncoupled in the optimization, but
currently there are no clinical consensus regarding the optimal approach. Combining
the uncertainties will potentially lead to unnecessary high doses to organs at
risk (OAR). On the other hand, the RO does not take anatomical changes and e.g.
flexion or rotation into account.
In this study we evaluated coupled
vs. uncoupled uncertainty scenarios in RO IMPT plans in head and neck cancer (HNC)
patients with respect to normal tissue complication probability (NTCP) and
robustness against re-planning.
Material and Methods
21 consecutive
oropharyngeal HNC patients treated with IMPT were selected. They were treated
with 3 dose levels: 66-68/60/50Gy in 33-34fx using 4-7 fields and a 5cm range
shifter. The clinical plans were optimized using robustness parameter
combinations of setup uncertainty of ± 4mm in all cardinal directions and ±
3.5% range uncertainty - 14 coupled scenarios in total. New plans were re-optimized
for similar target coverage with uncoupled robustness parameters - 8 uncoupled scenarios
in total.
The difference
in NTCP of ≥ Grade 2 dysphagia and ≥ Grade 2 xerostomia for the two RO
approaches were recorded.
Fifteen of 21
patients had been re-planned during the treatment course (median fx11 (range:
fx7-fx24)) due to insufficient target coverage. On the re-plan CT the target
coverage from the two RO approaches was compared on size of largest cold spot volume
and DVH parameters. Six of 21 patients were not re-planned and target coverage
was compared on the last control CT in the final week of treatment.
Test for significant
difference (p<0.05) were performed with Wilcoxon signed-rank test.
Results
For initial
planning the uncoupled plans showed a significant lower NTCP of median -0.4% (range:
-1.2%;0.4%) for dysphagia and median -0.2% (range: -1.1%;0.2%) for xerostomia
compared to the coupled scenarios.
Figure 1
shows the absolute size of the largest connected cold volume receiving less
than 95% of the prescribed dose for the 3 CTV's when the nominal plans were
re-calculated on re-plan CT or last control CT. The underdosage was significantly
larger for the uncoupled RO.
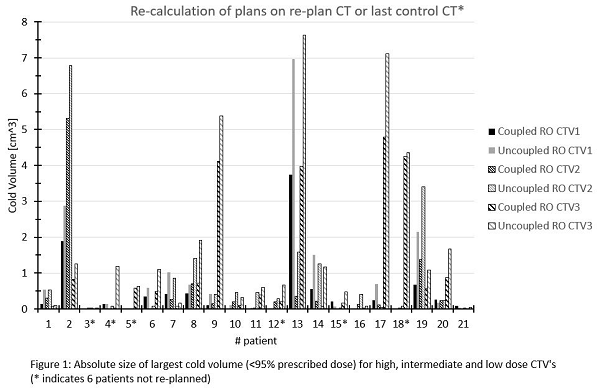
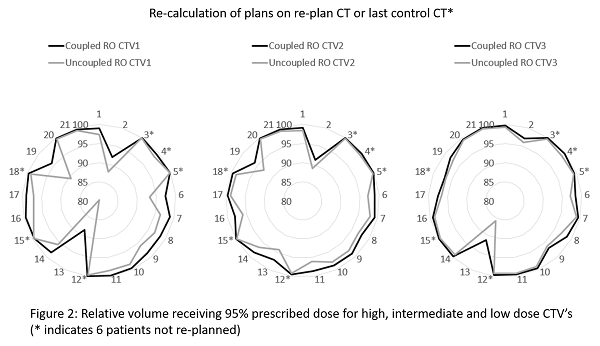
Figure 2 depicts the
relative volume receiving 95% of the prescribed dose from the re-calculation
taking range uncertainty into account (worst case of 2 scenarios).
Conclusion
Initial planning with uncoupled RO yielded lower
NTCP due to lower OAR dose. However, the uncoupled RO plans were less robust to
anatomical changes requiring re-planning during the treatment course. Contemporary planning is
not optimal as the probable scenarios of anatomical changes is not incorporated
in the treatment planning systems, but using the improbable combination of
uncertainty scenarios compensate somewhat for this.