Reproducibility and stability of spirometer-guided DIBH in left-breast radiotherapy
PO-1703
Abstract
Reproducibility and stability of spirometer-guided DIBH in left-breast radiotherapy
Authors: Pietro Viola1, Maurizio Craus1, Carmela Romano1, Gabriella Macchia2, Mariangela Boccardi2, Marica Ferro2, Vincenzo Picardi2, Donato Pezzulla2, Luca Indovina3, Milly Buwenge4, Silvia Cammelli4, Vincenzo Valentini5, Alessio Giuseppe Morganti4, Francesco Deodato2, Savino Cilla1
1Gemelli Molise Hospital, Medical Physics Unit, Campobasso, Italy; 2Gemelli Molise Hospital, Radiation Oncology Unit, Campobasso, Italy; 3Fondazione Policlinico Universitario A. Gemelli, Medical Physics Unit, Roma, Italy; 4IRCCS Azienda Ospedaliera Universitaria di Bologna, Radiation Oncology Unit, Bologna, Italy; 5Fondazione Policlinico Universitario A. Gemelli, Radiation Oncology Unit, Roma, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Deep inspiration breath-hold radiotherapy has
become a standard of care for left-sided breast cancer patients. We used
a surface guided optical system to quantify the reproducibility and stability
of spirometer-guided breath-hold breast treatments.
Material and Methods
Five
consecutive left-sided breast cancer patients were treated in breath-hold using
the Active Breathing Coordinator spirometer (ABC). Patients were treated with an
hybrid-IMRT technique and simultaneous integrated boost to surgical cavity. An
optical surface-guided scanning system device (AlignRT) was used to
continuously monitor the left breast during treatment. The inter-fraction,
intra-fraction and intra-breath-hold motion was quantified in the
anterior-posterior (VER), superior-inferior (LNG) and lateral-lateral (LAT)
directions. The DIBH intra-breath-hold
stability (S) was defined as the linear amplitude deviation during a DIBH
maneuver (and calculated as the gradient of the regression straight line
multiplied with the DIBH-time interval). For each breath-hold sequence during a
treatment fraction, the intra-fraction reproducibility (R) was defined as the
maximum difference between different DIBH levels. The inter-fraction
reproducibility (T) was determined as the difference between the mean
breath-hold level per fraction and the mean breath-hold level during the first
fraction. Correlations between ABC tidal volume and surface imaging deviations
were investigated.
Results
Each
treatment fraction was completed using 4-6 breath-holds. 75 treatment fractions
and 625 breath-holds during beam-on time were analyzed. Overall ABC
intra-session lung volume variation was <1.5%. With regard to
intra-breath-hold stability, the median linear deviations S were 1.3 mm
(95%-CI: [0.0–2.2] mm), 2.4 mm (95%-CI: [0.3–6.7] mm) and 0.8 mm (95%-CI: [0.0–1.7]
mm) ) in the VER, LNG and LAT directions, respectively. Results for the LNG
direction indicated that the drift over time during breath-hold are not
negligible, up to 9 mm even at constant inspired volumes. With regard to
intra-fraction reproducibility, the averaged results reported R median values of
1.3 mm (95%-CI: [0.0–1.9]
mm), 1.4 mm (95%-CI: [0.0–2.9] mm) and 0.8 mm (95%-CI: [0.0–1.3] mm) in the VER,
LNG and LAT directions, respectively. Median inter-fractional reproducibility
was found 0.0 mm (95%-CI: [-0.6–0.6] mm), -0.3
mm (95%-CI: [-1.4–0,2] mm) and 0.0 mm (95%-CI: [-0.2–0,2] mm) in the VER, LNG
and LAT directions, respectively. No
correlations were found between ABC breath-hold levels and surface monitoring deviations in all directions. Figure
shows an example of the ABC spirometer (upper) and AlignRT time trajectories
along VER and LNG directions (lower) for
three representative breath-holds. 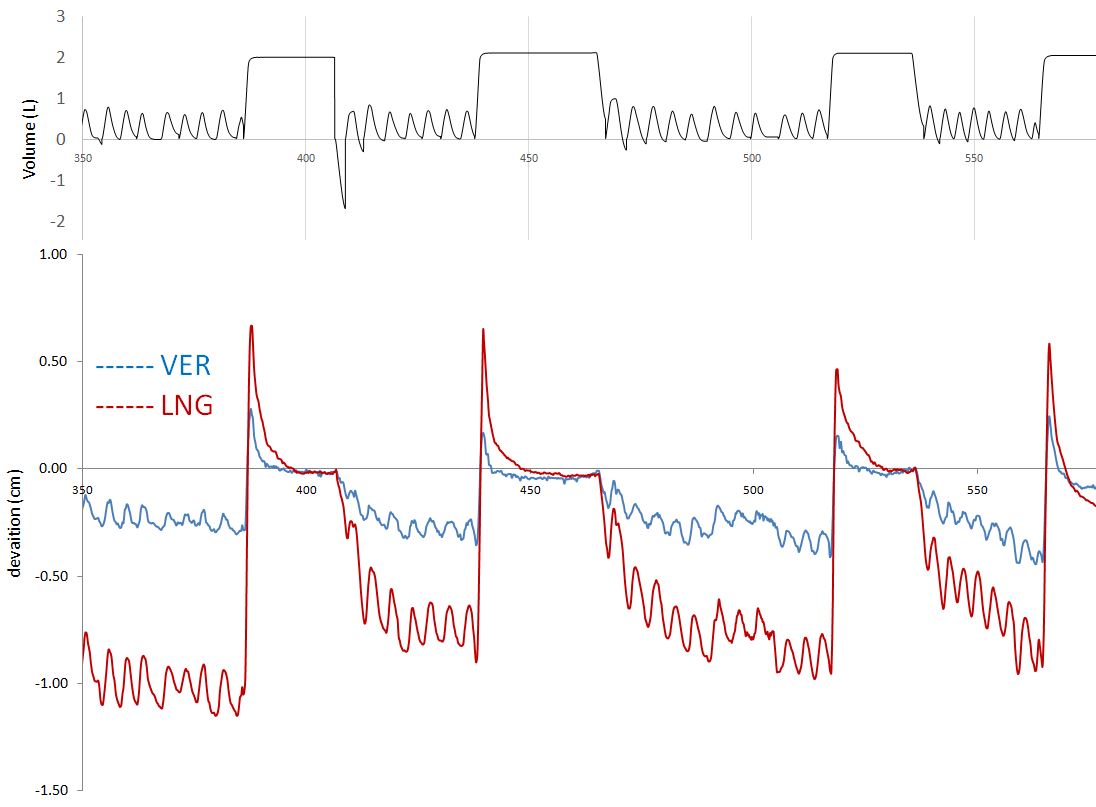
Conclusion
Despite
the use of spirometer-controlled lung volume, breast immobilization may not be
stable and reproducible as expected. The integration of spirometry with an optical
surface-guided guidance system may increase surface position reproducibility
during repeated DIBHs.