Fast delivery of IMRT to metastatic disease without planning CT simulation.
Koen Nelissen,
The Netherlands
PO-1684
Abstract
Fast delivery of IMRT to metastatic disease without planning CT simulation.
Authors: Koen Nelissen1, Eva Versteijne1, Suresh Senan1, Ben Slotman1, Wilko Verbakel1
1Amsterdam UMC, Radiation Oncology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy (RT) is an effective treatment for metastatic
disease. Fast treatment is desirable for patients requiring pain control and results in shorter interruptions of any systemic treatments. However, significant delays
can arise if a dedicated planning CT-scan (pCT) has to be scheduled before target
contouring and treatment planning is performed. Most patients have a recent diagnostic
CT-scan or PET-CT scan available but patient positioning and tumor expansion could
be different during RT-delivery. We developed a workflow for palliative patients that
involved performing pre-planning
on available diagnostic CTs (dCT), and subsequently
used plan adaption to account for any changes in target anatomy changes using a
cone-beam CT-scan (CBCT) prior to RT-delivery. This retrospective study assessed the feasibility of this workflow.
Material and Methods
Fifteen patients were selected from the hospital
database based on the following criteria: palliative treatment of metastatic
disease to the spine or ribs (1x8Gy), time between a dCT and pCT of <6 weeks
and CTV and OARs visible on dCT. Images from the selected patients were
analyzed in the Ethos platform (Varian Medical Systems), where the full
treatment workflow from treatment planning (TP) up until TP adaption on-couch
was emulated. The workflow involved the following steps; 1) contouring of
target and OARs on dCT by radiation oncologist (RO), with use of clinical PTV
margins (5mm); 2) treatment planning on dCT (TPref) according to
departmental guidelines (CTVV95%≥98%, PTVV95%≥95%) by a
researcher, reviewed by a medical physicist; 3) a RO reviewed the CBCT made
during treatment, and manually adapted contours if tumor progression was
visible. The RO also reviewed dosimetry of TPref on the daily
contours (TPd), followed by a final adapted plan of the day (TPa)
based on the on-couch anatomy on a CBCT. Treatment quality was analyzed by
comparing target coverage (PTVV95% and CTVV95%) and OAR
dose between the TPref , TPd and TPa.
Results
All TPa met clinical acceptance criteria. Minor
adaption of CTV, which was defined as contour adaptation in <4 slices, was
needed in 7 out of 15 patients, while major CTV adaption (edits in >4
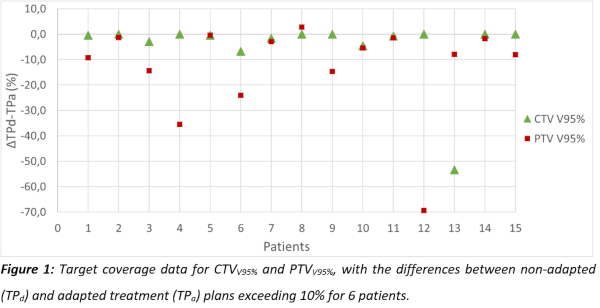
slices) were needed in 4 patients, and 4 patients required no CTV adaptions. Figure
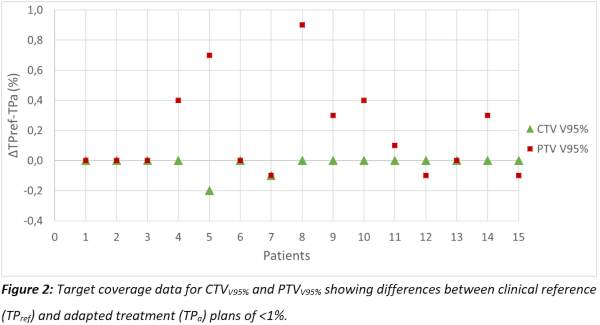
1 shows an improvement in target coverage in the TPa versus TPd,,
while achieving similar target coverage as TPref (Figure 2). Doses
delivered to OARs by the TPA were all within clinical acceptance
criteria, and differences seen were due to changes in target volume arising from
tumor progression between the dCT and treatment.
Conclusion
This study found that online adaption of palliative treatment
plans that were initially generated using dCTs, was feasible using on-couch
CBCT scans on the Ethos platform. We will now implement this workflow in our clinic,
with expected benefits in both departmental logistics and patient experience.