Monitor unit range check as an alternative for secondary dose calculation in online MR-guided RT
Danny Schuring,
The Netherlands
PO-1678
Abstract
Monitor unit range check as an alternative for secondary dose calculation in online MR-guided RT
Authors: Danny Schuring1, Roel Kierkels1, Guido Hilgers1, Ilona Potters1, Mariska den Hartogh2, Paul Jeene2, Kathrin Surmann1
1Radiotherapiegroep, Department of Medical Physics, Arnhem/Deventer, The Netherlands; 2Radiotherapiegroep, Department of Radiation Oncology, Arnhem/Deventer, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Currently there are no secondary dose calculations available that can accurately calculate dose in a magnetic field for an Elekta Unity system, the use of an monitor unit (MU)-range check was investigated as an alternative approach for detecting larger errors and outliers in treatment plans. This check is part of a comprehensive QA framework where QA procedures are integrated in the entire MR-linac workflow to have an efficient and effective method for detecting errors.
Material and Methods
A treatment procedure was developed for the hypofractioned treatment of prostate cancer patients on a Unity MR-linac (Elekta AB, Stockholm) using 5 fractions of 7.25 or 7.00 Gy. Treatment planning was performed in Monaco 5.40 (Elekta AB, Stockholm) using a class solution with strict guidelines on IMRT parameters and variation of planning objectives. Checks on features essential for the dose calculation and optimization, such as density overrides and adaptation type, were integrated in the online adaptive workflow. The number of MUs of the online fraction plan was compared to the pre-treatment plan and previous fractions of the patient prior to online treatment delivery. The number of MUs and other plan characteristics were collected for 23 clinical patients for both the pre-treatment as well as the online adapted treatment plans. Pre-treatment QA measurements of the plans were performed using an Octavius 1500MR array (PTW, Freiburg).
Results
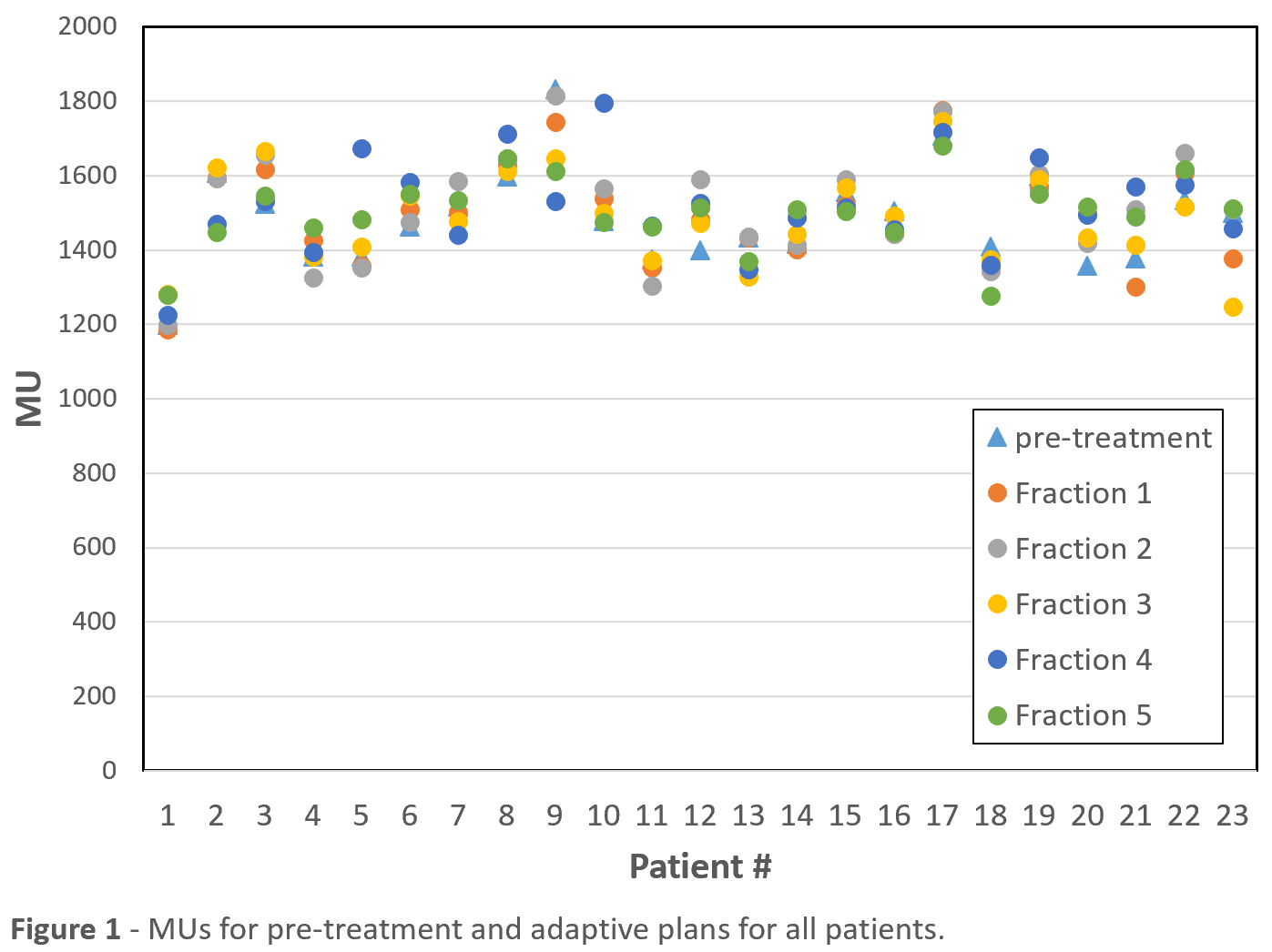
The average
number of MUs in the pre-plan was 1485 ± 132 (1 SD). Figure 1 shows the number
of monitor units of the pre-treatment plan as well as the treatment fractions
for all 23 patients. No statistically significant difference was found between
the average number of MUs over all adaptive plans of all patients (1501 ± 130 MU)
and the pre-plan average. Inter-fraction variation of the number of MUs was
reduced compared to the inter-patient variation (average SD of 62 MUs). For 14
of the 23 patients, this variation was below 3% of the total number of MUs compared
to the pre-treatment plan. A larger inter-fraction variation correlated with
larger variations in patient anatomy (bladder and rectal filling). No
correlation was found between the number of MUs and the number of segments in
the treatment plan.
Pre-treatment QA measurements of the treatment plans had a pass rate above 98.5% (median 100%), and an average mean gamma of 0.397 (2%/2mm local gamma criterion). No correlation was found between the mean gamma and the number of MUs for the plan.
Conclusion
An efficient and effective QA procedure was developed for online adaptive MR-guided treatment of prostate cancer patients. The MU range check can be used in combination with a strict class solution and integrated QA checks of the online adaptive workflow. The inter-patient variation of MUs is limited, and the intrapatient variation between different fractions is further reduced. An MU range check can thus be used for detecting outliers as an alternative to a secondary dose calculation.