Two-fraction prostate radiotherapy using high field MR-linac: technique and initial experience
Robert Adam Mitchell,
United Kingdom
PO-1662
Abstract
Two-fraction prostate radiotherapy using high field MR-linac: technique and initial experience
Authors: Robert Adam Mitchell1, Stefanos Diamantopoulos1, Alex Dunlop1, Sophie Alexander2, Edmund Goodwin1, Trina Herbert2, Sarah Jones3, Jonathan Mohajer1, Simeon Nill1, Gillian Adair Smith2, Rosalyne Westley2, Uwe Oelfke1, Alison Tree2
1The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust, Joint Department of Physics, London, United Kingdom; 2The Royal Marsden NHS Foundation Trust, Radiotherapy, Sutton, United Kingdom; 3The Royal Marsden NHS Foundation Trust and the Institute of Cancer Research, Radiotherapy, Sutton, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The HERMES trial (NCT04595019) is
investigating the feasibility and safety of delivering prostate SBRT in two
fractions (2#) compared to five using the Unity MR-linac platform (MRL, Elekta
AB, Stockholm). We report on the 2# treatment workflow and the dosimetric
results for the first recruited patient, who was randomised to the 2# trial arm.
Material and Methods
For 2#, the target structures and dose levels (cGy) are:
- GTVpb_2700: intraprostatic lesion
- PTVpsv_2400: 3mm isotropic expansion of prostate including
1cm of seminal vesicles (SVs)
- PTVsv_2000: 3mm isotropic expansion of prostate including
1-2cm SVs, depending on patient risk
Treatment planning is performed using the Monaco v5.40.01
(Elekta) treatment planning system and consists of 11-field IMRT. PTV dose
coverage is systematically reduced around rectum and bladder to achieve the
mandatory dose constraints. Plans are adapted online via the Adapt-to-Shape
workflow (ATS), with any post-ATS planning prostate baseline shifts corrected
using Adapt-to-Position (ATP). Due to the extended beam-on time for 2# and
absence of clinically-available real-time adaptive planning tools, each
fraction is split into two sub-fractions (sub-#) which are treated as two
separate ATS workflows, delivered back-to-back on the same day. Patients will
leave the treatment room between sub-# for bladder re-preparation.
For the first patient, to estimate target and OAR doses at
the time of treatment, the clinically delivered treatment plans for each sub-#
were re-calculated offline on the MRL MRI scans (T2-weighted) acquired at the
time point closest to beam-on. OAR doses were accumulated over the entire
treatment course by averaging their respective calculated dose statistics
across all sub-fractions.
Results
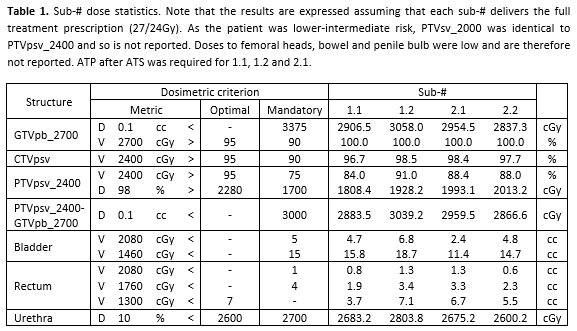
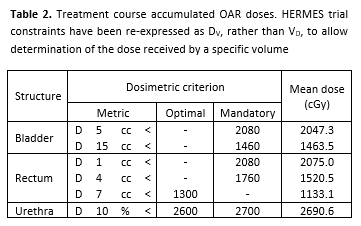
Individual sub-# results are
given in Table 1. Treatment course mean OAR doses are given in Table 2. Whilst
OAR dose constraints were exceeded on individual sub-#, the simple dose
accumulation suggests that OAR doses were within their mandatory constraints
for the overall treatment course, with the bladder D15cc being the only
exception. However, this dose accumulation approach is conservative and assumes
that the same OAR regions received the highest doses on all sub-#. Hence this
is likely an overestimation of dose.
The total times to complete each
# were 2.2hr and 1.6hr respectively. Whilst both were within the allocated
2.5hr treatment slot, #1 was longer than expected due to necessary management
of rectal distension and a Monaco dose calculation failure.
Conclusion
We have implemented a workflow on
the Unity MR-linac for HERMES trial two-fraction prostate SBRT and successfully
treated the first patient whilst predicting to maintain OAR doses over the
course of treatment. A sub-fraction workflow approach was followed to reduce
prostate motion during treatment. It is expected that this sub-fraction
approach will become redundant once real-time online adaptive planning using
MLC tracking is clinically available.