Accuracy of diffusion-weighted MRI in radiotherapy setup for multicenter PET/MRI in head/neck cancer
PO-1656
Abstract
Accuracy of diffusion-weighted MRI in radiotherapy setup for multicenter PET/MRI in head/neck cancer
Authors: René Mario Winter1, Maren Lium2, Ola Engelsen3, Oddbjørn Sæther4, Kathrine Røe Redalen2
1Norwegian University of Science and Technology, Department of Physics , Trondheim, Norway; 2Norwegian University of Science and Technology, Department of Physics, Trondheim, Norway; 3University Hospital of North Norway (UNN), PET Imaging Center, Tromsø, Norway; 4St. Olavs hospital, Trondheim University Hospital, Department of Radiology and Nuclear Medicine, Trondheim, Norway
Show Affiliations
Hide Affiliations
Purpose or Objective
Diffusion-weighted MRI (DWI) is of growing interest in multicenter imaging biomarker studies. However, using different MR systems in multicenter studies has the drawback that it may increase the variation in the image values. This is especially relevant for PET/MR systems tailored to imaging the patient in radiotherapy position, since the MR coil setups designed to accommodate the patient positioning tools typically have lower signal-to-noise ratio (SNR) which may add even more variation. Our aim was to assess the performance of a radiotherapy tailored PET/MR system for quantitative DWI in a multicenter imaging study in head/neck cancer (EMINENCE, clinicaltrials.gov NCT04612075).
Material and Methods
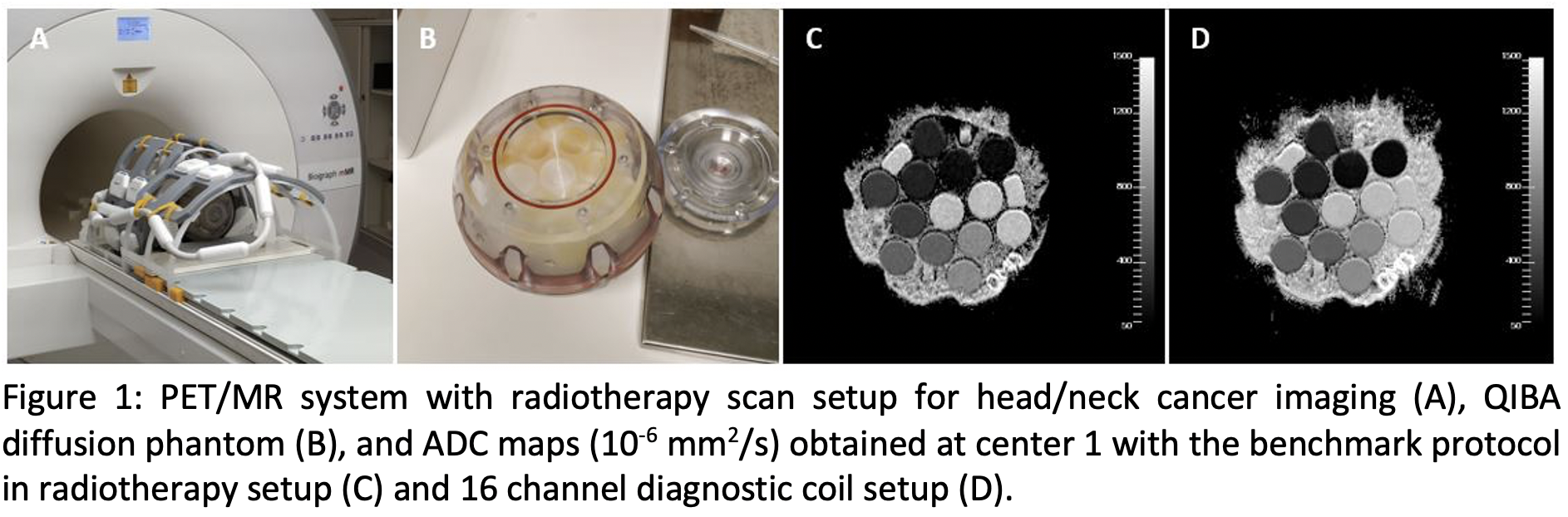
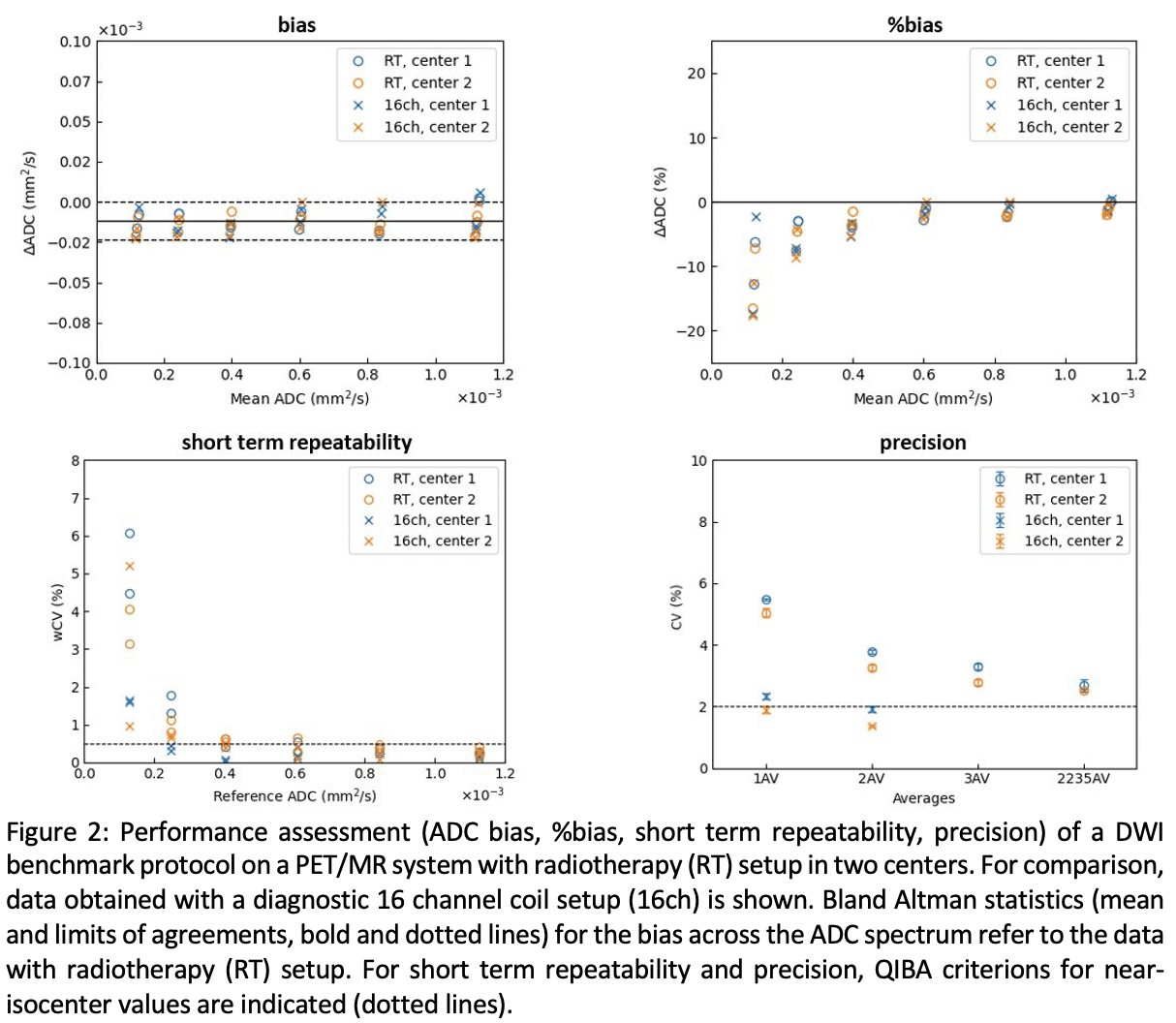
Performance was assessed on a 3T PET/MR system (Siemens) with radiotherapy setup (Medibord; Fig. 1A) in two different centers. DWI was measured in a calibration phantom (High Precision Devices, Inc; Fig. 1B) recommended by the Quantitative Imaging Biomarkers Alliance (QIBA). The ice water cooled phantom contained 13 vials of different mediums to allow the measurement of six known apparent diffusion coefficients (ADC). For a set of four scans the QIBA benchmark protocol (SS-EPI; four b-values; 0, 500, 900, 2000 s/mm2; 1 average each; transverse acquisition) was used. Scans were repeated three times using the same protocol but with increasing number of averages (2; 3; 2,2,3,5) to account for the reduced SNR in radiotherapy setup and investigate possible improvements in ADC accuracy. SNR of the b0 image, ADC bias (ΔADC, measured minus true value), %bias, precision (coefficient of variation, CV), short-term repeatability (within-subject CV, wCV) and intercenter reproducibility (iCV) were analyzed according to the QIBA profile. Measurements were repeated with a diagnostic 16 channel coil (16ch) for comparison. A clinical protocol for low distortion DWI (RESOLVE) was tested in center 1.
Results
ADC maps with radiotherapy and 16ch diagnostic coil setups are shown in Fig1. C-D. Compared to the 16ch coil, SNR with radiotherapy setup was lower by a factor of 2.5 (b0 image, near isocenter) but still met the QIBA criterion (SNR>50). Regarding ADC accuracy with radiotherapy setup in center 1 and 2 (Fig. 2), the bias was -0.06 (±0.07) and -0.18 (±0.06) x10-4 mm2/s; precision was 5.4% and 4.9%; short term repeatability error was 0.3% for both centers. The intercenter reproducibility error was 0.6%. Thus, all QIBA criterions for ADC were met near isocenter except precision. ADC %bias and repeatability were worse in the very low ADC range. ADC precision could be improved by increasing number of averages. Similar results were obtained with the clinical RESOLVE protocol (bias, -0.04 (±0.04) x10-4mm2/s; precision, 3.2%; repeatability, 0.2%).
Conclusion
Measurement of consistent ADC values on a PET/MR system with radiotherapy setup is feasible at different centers, meeting most QIBA criterions in phantoms. Stable results were obtained with the clinical RESOLVE protocol in a multicenter imaging study.