Treatment planning protocol in Single-Dose Radiation Therapy for prostate cancer
PO-1645
Abstract
Treatment planning protocol in Single-Dose Radiation Therapy for prostate cancer
Authors: Denis Panizza1,2, Raffaella Lucchini3,2, Valeria Faccenda1,4, Paolo Caricato1,4, Elena De Ponti1,2, Stefano Arcangeli3,2
1ASST Monza, Medical Physics Department, Monza, Italy; 2University of Milan Bicocca, School of Medicine and Surgery, Milan, Italy; 3ASST Monza, Radiation Oncology Department, Monza, Italy; 4University of Milan, Department of Physics, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Great
emphasis on rigorous planning and delivery techniques must be placed when using
extreme hypofractionated regimens to fully exploit their potential benefits in
optimizing the therapeutic ratio, thus yielding excellent clinical outcomes. The
aim of this study was to report the clinical treatment planning implementation for
organ-confined linac-based prostate
Single-Dose Radiation Therapy (SDRT) using electromagnetic tracking for
real-time intrafraction organ motion management (NCT04831983).
Material and Methods
Since
June 2021 five patients with localized unfavorable intermediate or selected
high-risk prostate tumors were enrolled to receive an ultra-high SDRT of 24 Gy
(BED 1.5 = 408 Gy). Patients were simulated with empty rectum and bladder
filled by a Foley catheter. Fused CT and T2W 3D MRI image sets were used to
delineate target and OARs. The PTV consisted of the CTV with a 2-mm isotropic margin.
A high-dose avoidance zone (HDAZ) was created by a 3-mm expansion around the rectum,
bladder, and urethra. Patients were planned to a minimum dose defined by the
OARs dose constraints with a dose escalation to 24 Gy to the target volume away
from the HDAZ. A 10MV FFF beam energy single arc from 140° to 220° was
optimized using target penalties
with the Monaco Monte Carlo TPS. During the treatment delivery, CBCT matching ensured
patient setup alignment and target localization, and any online tracking detected motion greater than 2 mm was realigned by
repeating CBCT.
Results
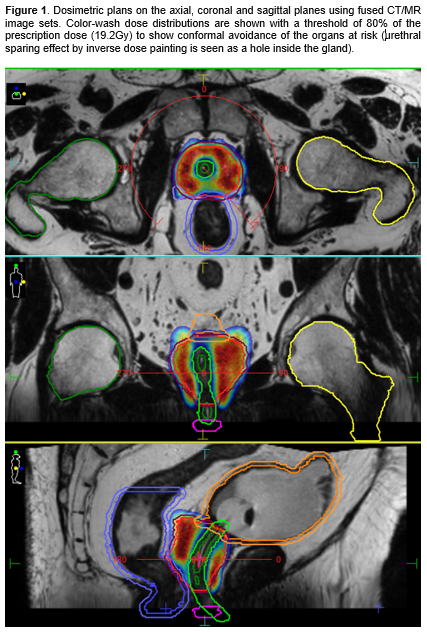
Figure
1 shows axial, sagittal,
and coronal fused CT/MR slices representing the dose distribution for a patient
treated with a single fraction of 24 Gy. Treatment goals and characteristics
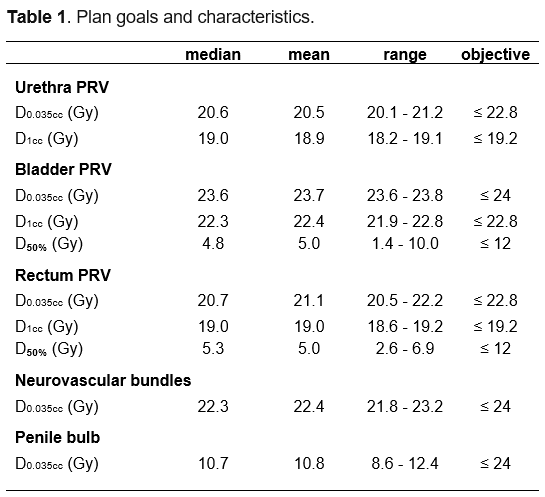
are summarized in Table1. All the predefined planning objectives were
fulfilled. Average PTV volume was 57.1 cc (range 25.6-78.8). Average beam
delivery time lasted 4.5 ± 0.6 minutes. Average total monitor units per plan
were 6709 ± 525. All the treatment plans were quality assured using a two-dimensional
array with silicon diodes and fulfilled the gamma (2%/2mm) passing rate >90%
objective.
Conclusion
The
use of an HDAZ during planning limited the volume of rectal mucosa receiving critical
doses. The accomplishment of urethral sparing via negative dose-painting to
minimize genitourinary toxicity is feasible through appropriate imaging
procedures and online tracking during treatment delivery. Our preliminary
findings offer encouraging perspectives on the feasibility and safety of 24 Gy
SDRT in organ-confined prostate cancer.