Feasibility of low-dose 4DCBCT for patient setup and motion measurement
Josh Lindsay,
United Kingdom
PO-1631
Abstract
Feasibility of low-dose 4DCBCT for patient setup and motion measurement
Authors: Josh Lindsay1, Abigail Bryce-Atkinson1, Simon Meara2, Corinne Faivre-Finn1, Cynthia Eccles2, Marianne Aznar1, Marcel van Herk1
1The University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom; 2The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
4DCBCT can improve dose delivery in patients with mobile
tumours. However, in some populations, there may be concerns over dose burden –
e.g. in younger patients with longer life expectancy. Here we explore the
possibility of low-dose 4DCBCT by assessing CBCT-CT registration accuracy and
tumour motion amplitudes in simulated low-dose images using clinical dose level
scans as reference.
Material and Methods
4DCBCT scans of 5 lung SABR patients with tumour motions of 11
-19mm were acquired as part of routine treatment using 2-4 minutes scan time,
120 kV, 650-1300 projection images, 0.32mAs per projection image, CTDI 5.6-11.2mGy.
Low-dose images at 30% and 10% of clinical dose were simulated, resulting in
the same or lower dose as corresponding 3DCBCT modes. Low-dose scans were
simulated by adding non-uniform Gaussian noise to the original projection data,
informed by the signal-noise relationship measured in phantom images.
Dual-registration from 4DCBCT to average 4DCT was performed at each dose level,
first registering the spine based on gray value in a region of interest (ROI) around
the vertebrae and then applying 4D tumour registration using ITV+5mm as an ROI.
Registrations at each dose were repeated 100 times with added random shifts
(SD=3mm in each direction) after spine registration to evaluate consistency
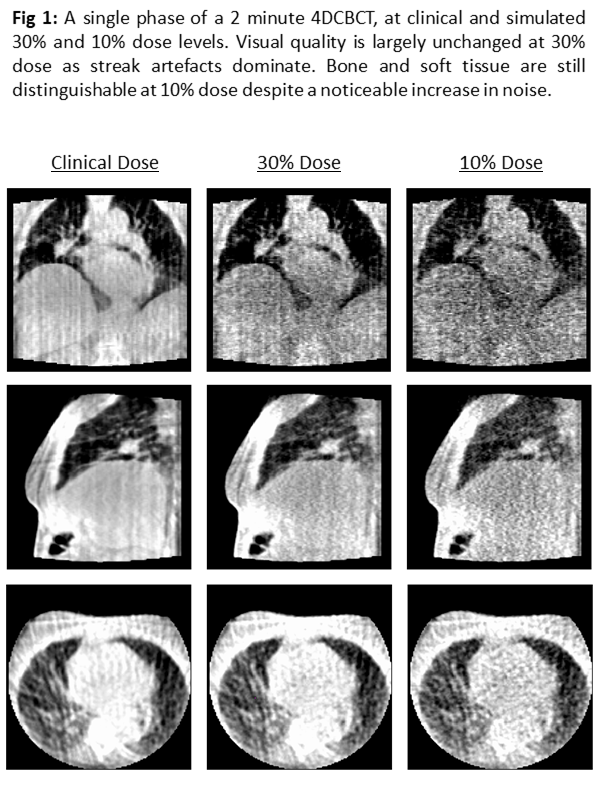
given realistic baseline shifts. For the 10% and 30% dose levels, image quality
was visually evaluated and relative accuracy compared to reference images
looking at 1) vector differences between couch shifts, 2) estimated motion
amplitude and 3) registration failure rate (error > 5mm). Mean couch and
motion vectors at clinical dose were taken as the gold standard for these comparisons.
Results
Visual image quality at 30% dose was comparable to full
dose, but 10% dose images were notably noisier (Fig 1). Automatic registration
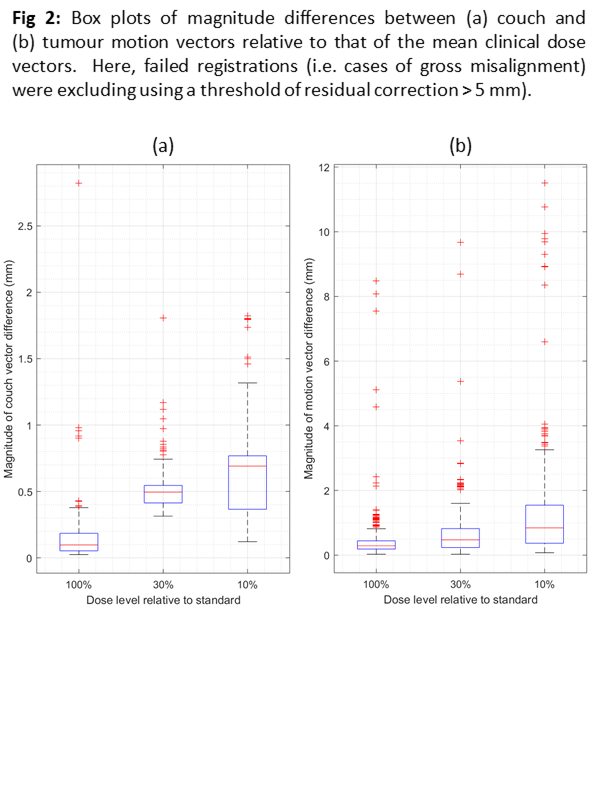
of each low-dose image remained consistent with that of the standard-dose. The
median, mean, and SD of magnitude of couch vector differences were 0.10mm, 0.14mm,
and 0.17mm at clinical dose; 0.49mm, 0.51mm, and 0.13mm at 30% dose; and 0.69mm,
0.62mm, and 0.28mm at 10% dose (Fig 2a). The magnitude difference in
measurement of the tumour motion vector gave values of 0.29mm, 0.37mm, 0.35mm for
clinical; 0.47mm, 0.59mm, and 0.49mm at 30% dose; and 0.81mm, 1.10mm, and 0.86mm
at 10% dose (Fig 2b). The registration failure rate at any dose level was below
2%.
Conclusion
Low-dose 4DCBCT has a minimal effect on automatic
registration accuracy and tumour motion estimates at 30% and 10% of clinically
used doses. Decreasing the dose to 30% did not have a considerable detrimental
effect on image quality, since the impact of streak image artefacts exceed that
of image noise at this dose level. This work highlights the feasibility of
reduced-dose 4DCBCT, which could be relevant for patients for whom 4DCBCT is
avoided due dose concerns. We show that using the same or lower dose than in clinical
3D modes is acceptable.