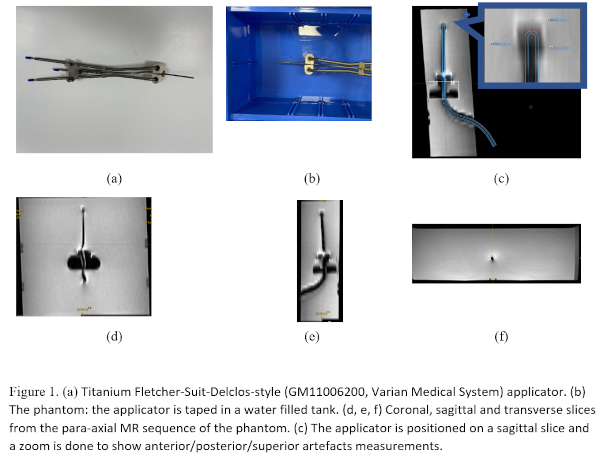
Titanium
Fletcher-Suit-Delclos-style (GM11006200, Varian Medical System) applicator set was
used in this study (Fig 1.a). It was placed in a water filled tank to simulate
a phantom (Fig 1.b) and scanned using the brachytherapy uterine protocol of our
clinic. The acquired images were sagittal T2 cube (a voxel size of 0.39 × 0.39
× 1.2 mm3, a matrix size of 512 × 512 × 232, a repetition time TR = 2000
ms, an echo time TE = 59.67 ms, and a flip angle FA = 90°), para-coronal T2
propeller (a voxel size of 0.5 × 0.5 × 3 mm3, a matrix size of 512 ×
512 × 15, TR = 1406.3 ms, TE = 82.08 ms, FA = 140°), para- axial T2 propeller
(a voxel size of 0.39 × 0.39 × 3.29 mm3, a matrix size of 512 × 512 × 51, TR = 5319.7
ms, TE = 95.9 ms, and FA = 140°) (Fig. 1. d, e, f).
The
tandem and ovoid geometries were projected from the Varian’s library of
applicators into the MRI and were positioned manually to their location in the
images by the physicist (Fig 1.c). A reference segmentation of the tandem was
therefore extracted. The tandem, which appear with low intensities (signal
loss), was segmented automatically on the MRI sequences by thresholding.
Dice,
sensitivity, and Jaccard indices were computed between the reference
segmentation and the MRI-based segmentation of the tandem in each MRI sequence.
Distances were measured from the tandem tip to the MRI artifact edge in right/left/superior
and anterior/posterior directions in the coronal and sagittal views
respectively. Eclipse Brachytherapy Planning System (Version 16.1) was used for
measurements.