Low-dose CT allows for accurate proton dose calculation in esophageal cancer
Masoud Elhamiasl,
Belgium
PO-1607
Abstract
Low-dose CT allows for accurate proton dose calculation in esophageal cancer
Authors: Masoud Elhamiasl1, Gilles Defraene2, Koen Salvo3, Edmond Sterpin2,4, Johan Nuyts1
1KU Leuven, Department of Imaging and Pathology, Division of Nuclear Medicine, Leuven, Belgium; 2KU Leuven, Department of Oncology – Laboratory of Experimental Radiotherapy, Leuven, Belgium; 3UZ Leuven, Department of Radiotherapy, Leuven, Belgium; 4UCLouvain, Institut de Recherche Expérimentale et Clinique, Molecular Imaging Radiotherapy and Oncology Lab, Brussels , Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Adaptive
proton therapy aims to deliver the radiation dose accurately in the presence of
anatomical changes by practicing a CT imaging feedback loop on a regular basis
to systematically monitor anatomical changes and adapt the treatment plan if
required. However, the series of these repeated CT scans results in an
accumulated additional patient dose, in particular, if 4DCT is performed to
account for breathing effects. We hypothesized that the signal-to-noise ratio
provided by conventional 4DCT protocols is higher than needed for proton
therapy dose calculation. In this study, we aim to assess the effect of
reducing CT dose on proton dose calculation in esophageal cancer.
Material and Methods
A
standard-dose 4DCT scan [Siemens SOMATOM Drive, 120 kVp, Q.ref mAs = 50 mAs, 10
breathing phases] for an esophageal cancer patient was used to investigate the
effect of CT dose reduction on proton dose calculation. Low-dose CTs (LDCTs) with
gradual reduction in dose were simulated using our in-house LDCT simulator.
Several phantom studies previously confirmed the accuracy of the simulated
images in providing realistic LDCT images.
An
intensity modulated proton therapy plan with two posterior beams (150˚ and
180˚) was generated in RayStation (Version 9B) with the average image of the standard-dose
4DCT as planning CT. The prescribed dose of 50.40 Gy RBE (28 fractions of 1.80
Gy RBE) was optimized on the iCTV using robustness settings of 7mm setup error
and 2.6% range error. To avoid additional variation due to the statistical
uncertainty of the Monte Carlo simulation, a pencil beam engine was used for
plan optimization and final dose calculation. The dose distributions were then recalculated for the LDCTs
using the optimized plan and the results were compared with that of the
standard-dose scan.
Results
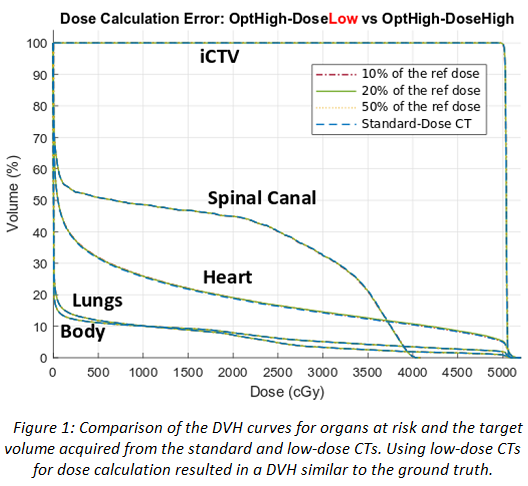
The dose
distributions on standard-dose CT and LDCTs were compared using the Dose-Volume
Histogram (DVH) and gamma index tests. Figure 1 compares the dose distributions
using the DVH curves of organs at risk and the target volume. The DVH curves
are on top of each other, indicating the similarity of the dose distributions.
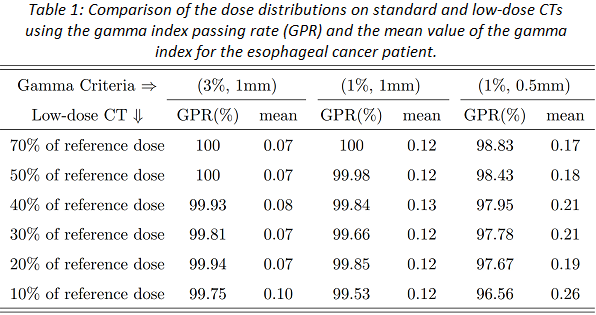
Table 1 shows the gamma passing rate of the dose distributions acquired from
LDCTs. It can be seen that the gamma passing rate decreases by reducing the CT
dose, however, it is always higher than 99.50% for a 1%/1mm criterion,
confirming the similarity of the dose distributions calculated on the
standard-dose and LDCTs.
Conclusion
Our results
on patient data suggested the possibility of reducing the CT dose for the
purpose of dose calculation during the course of treatment. An aggressive dose
reduction by a factor of up to 10 did not have a significant effect on the dose
distributions. A quantitative analysis utilizing more patient data is ongoing.