Weekly dosimetric evaluation of CBCT-based synthetic CTs for proton therapy of head & neck patients
Rutger de Koster,
The Netherlands
PO-1604
Abstract
Weekly dosimetric evaluation of CBCT-based synthetic CTs for proton therapy of head & neck patients
Authors: Rutger de Koster1, Adrian Thummerer1, Gabriel Guterres Marmitt1, Daniel Scandurra1, Hans Langendijk1, Stefan Both1
1University Medical Center Groningen, University of Groningen, Department of Radiation Oncology, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
In proton therapy it is common practice to
acquire weekly verification CTs to monitor treatment progress and recalculate
treatment plans on updated patient anatomy. For daily adaptive proton therapy
workflows however, repurposing in-room images such as cone-beam CTs (CBCT), is
more suitable since it is not adding to the clinical workload and does not
cause any additional dose burden to the patient. CBCT images, routinely
acquired for pre-treatment position verification, provide a daily
representation of the patient anatomy but suffer from severe imaging artefacts
preventing accurate dose calculations. Recently deep neural networks have shown
promising results to correct CBCT images and generate high quality synthetic
CTs (sCT), for proton dose calculations.
Therefore, the aim of this study was to compare
weekly rCT and daily sCT images of head and neck cancer patients to investigate
the dosimetric accuracy of CBCT-based sCTs generated by a neural network.
Material and Methods
A dataset of 30 head and neck cancer patients
was utilized to generate synthetic CTs from daily pre-treatment patient
alignment CBCTs using a previously developed and trained UNet deep
convolutional neural network. Afterwards, clinically used proton treatment
plans were recalculated on sCTs and weekly rCTs to evaluate the dosimetric
accuracy of sCTs. Dose to clinical target volumes (CTV) and selected
organs-at-risk (OAR) were compared between pCTs and both weekly rCTs and
same-day sCTs by calculating mean dose differences. The investigated
organs-at-risk include submandibular glands, pharyngeal constrictor muscles,
parotid glands and the oral cavity.
Results
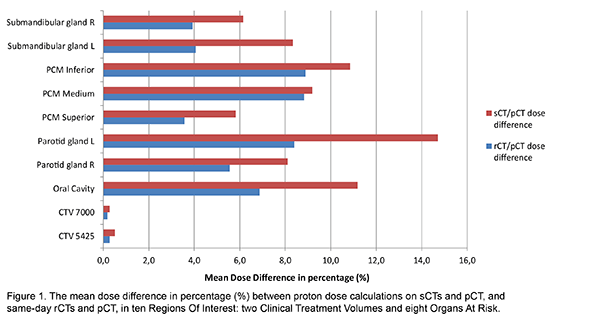
Figure 1 shows the mean relative dose
differences between sCT/pCT and rCT/pCT pairs per ROI. The best agreement
between pCT and rCT/sCT was observed for the low dose CTV (CTV 5425) with mean
dose difference values of 0.3±0.2 % [0.18±0.15 Gy](rCT) versus 0.5±0.7 % [0.32±0.45
Gy](sCT), and for 0.2±0.2 % [0.13±0.11 Gy](rCT) versus 0.3±0.2 % [0.19±0.16 Gy](sCT)
for the high dose CTV (CTV 7000). For all OARs, significantly larger dose
differences were found than for the CTVs. The largest difference between sCT and
pCT doses were observed in the left parotid gland with 14.7±16.4 % [1.61±1.31
Gy], compared to 8.4±9.2 % [1.01±0.87 Gy] between rCT and pCT, and in the left submandibular
gland with 4.1±5.3 % [1.32±1.37 Gy](rCT) compared to 8.3±11.6 % [2.43±2.69 Gy](sCT).
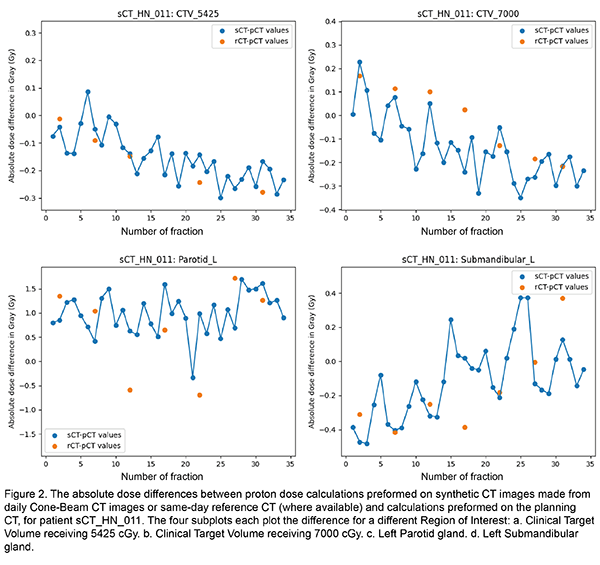
Overall, rCTs showed lower dose differences for all regions of interest. Figure
2 shows a comparison of daily sCT/pCT and weekly rCT/pCT dose differences for
target volumes and OARs of the entire treatment of an exemplary patient.
Conclusion
The
deep learning based sCTs showed high agreement for target volume doses (<1%).
However, larger dose differences were observed at OAR level. Further studies
are required to investigate if these dose differences are clinically acceptable
and if CBCT- based sCTs can fully substitute rCTs in the future.