The use of LEGO to assess CT-MRI fusion accuracy for stereotactic radiosurgery
Geoff Heyes,
United Kingdom
PO-1594
Abstract
The use of LEGO to assess CT-MRI fusion accuracy for stereotactic radiosurgery
Authors: Geoff Heyes1, Rob Flintham2, Hannah Augustus1, Ruth Stange1
1Queen Elizabeth Hospital Birmingham, Radiotherapy Physics, Birmingham, United Kingdom; 2Queen Elizabeth Hospital Birmingham, Medical Physics, Birmingham, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Magnetic Resonance (MR) at 3T
used to define targets for stereotactic radiosurgery (SRS) treatments. Images
are fused to Computed Tomography (CT) for treatment planning. The delivery accuracy
of the CyberKnife system is <1mm. MR images can suffer spatial distortions >1mm,
and can be highly variable according to the local MR equipment, protocols and
patient setups. For small targets (<0.5cc), or in multiple brain metastases
where accurate fusion across the whole brain is required, it is critical to
assess these distortions locally and their impact on dosimetric accuracy for
SRS.
Material and Methods
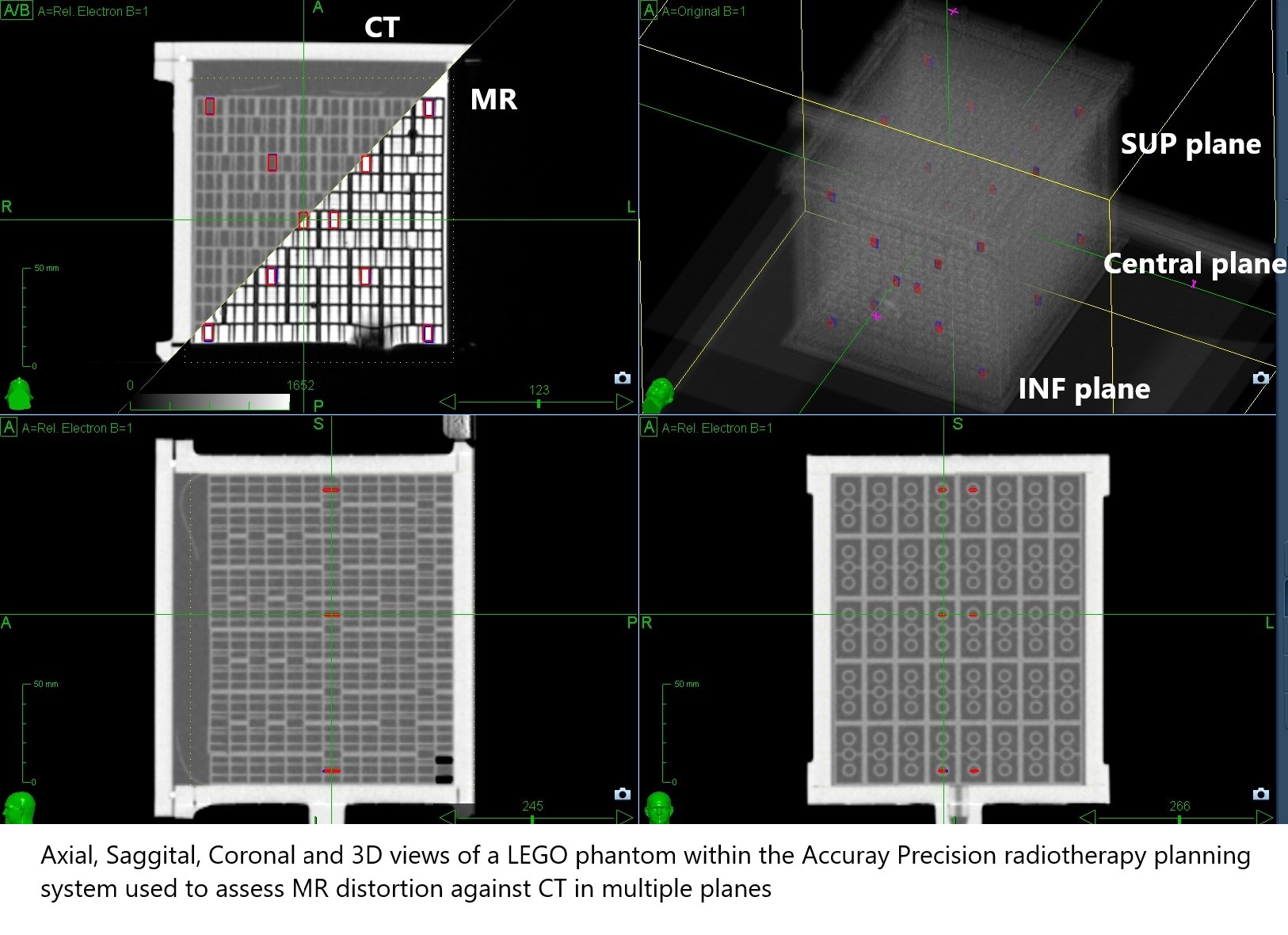
A phantom was made using 520 LEGO (Billund, Denmark) bricks with each
brick manufactured to a tolerance of 20µm. The resulting cuboid (125mm x 126mm x 160mm) of
similar dimensions to a human brain was encased in a custom-made Perspex phantom
filled with food-grade mineral oil to give a uniform MR signal at 3T. The cuboid was scanned on a Siemens Skyra 3T MR (Erlangen, Germany) using our
standard-of-care SRS planning sequence, and on a 1mm Philips CT. Further MR scans were
performed with the centre of the phantom offset in 16mm steps (equivalent to 1
Lego brick width) from the centre of the MR bore in the Sup-Inf plane to
maximum offset of 64mm. Each MR dataset was fused to CT using the Accuray
Precision radiotherapy planning system. This software was used to assess the
displacement of 30 bricks from the true position as defined by CT.
Results
LEGO provided the ability to construct a highly uniform phantom to
assess the geometric accuracy of CT-MR fusion across a volume similar to that
used for intracranial SRS. When the phantom was correctly aligned to MR
isocentre; the accuracy was <1mm centrally and <2mm at slices +/-80mm Sup-Inf.
A 32mm Sup-Inf offset from MR isocentre resulted in distortions of <4mm at
the edges but remained <1mm centrally. The accuracy in the central region was
maintained even when the phantom was offset 64mm from the MR isocentre, but became
significantly worse at the phantom edges, with distortions up to 7mm. These
edge distortions would be significant, since typical dose gradients of up to
7Gy/mm can be achieved in SRS. For multiple targets, the isodose distribution
is rarely spherical; in these cases, along certain planes the dose gradient may
only be 2Gy/mm. The scanner’s default distortion correction filters were able
to correct the extreme edge distortions to <1 mm, but with a loss of MR resolution.
Conclusion
This study highlights the ability to accurately assess
CT-MR fusion accuracy for SRS with a LEGO phantom. For patients with multiple metastasis,
additional care should be taken if there are lesions at extremes of the
dataset. Good MR isocentric positioning of the patient and the use of
distortion correction filters reduce these effects, and enables treatment of
all lesions with good dosimetric precision. If patient alignment is not ideal there
is a risk of significantly under-dosing peripheral targets due to the steep
dose gradients used within SRS.