Gating Device L: an external surrogate for respiratory motion tracking on TrueBeam
Mette Marie Bruun Nielsen,
Denmark
PO-1589
Abstract
Gating Device L: an external surrogate for respiratory motion tracking on TrueBeam
Authors: Mette Marie Bruun Nielsen1, Nikolaj Kylling Gyldenløve Jensen2, Sidsel Marie Skov Damkjær3
1Zealand University Hospital, Oncology and Palliative Care, Næstved, Denmark; 2Rigshospitalet, Oncology, Copenhagen, Denmark; 3Herlev and Gentofte Hospital, Oncology, Herlev, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients with breast cancer treated in deep
inspiration breath
hold with external beam radiotherapy require a motion management (MM) system.
The gating system for TrueBeam from Varian provides MM with an external
surrogate. When an external surrogate is used for MM, placing it closer to the
breast increases the precision of the tracked target motion (Skyttä et al. Acta
Oncol. 2016;55:970-75). However, placing the surrogate closer to the target may
result in the treatment beams going through the surrogate thus causing an
unintended bolus effect. It is therefore crucial that the design of a surrogate
minimizes the bolus effect to allow for placement near the breast. In this
study, we have tested a new surrogate: Gating Device L (GDL) and compared it to
Varian’s Truebeam reflector block (RB), as well as a modified version of the
reflector block (MRB) (see figure 1), with respect to surface dose, bolus
effect and tracking capabilities.

Figure 1: The three
surrogates investigated: The Gating Device L (GDL, the Reflector Block (RB) and
the Modified Reflector Block (MRB).
Material and Methods
Percentage depth dose
curves and profiles with and without surrogates were measured with Gafchromic
film and performed in-silico in the treatment planning system (TPS) to assess
the surface dose and bolus effect in a 6 MV beam. RB and GDL were compared in
the TPS to evaluate the dosimetric foot print on dose distributions on a static
field directly through the surrogates and by the Volumetric Modulated Arc
Therapy (VMAT) technique and compared by calculating the Dice Similarity
Coefficient (DSC). The tracking capabilities of RB and GDL by the gating system
were investigated with induced pitch, roll and yaw of the surrogates.
Results
Surface dose was increased up to 295%, 277%
and 190% for RB, MRB and GDL respectively compared to no surrogate with GDL
having a smaller physical surface area of 11 cm2 compared to 60 cm2
of RB and MRB (see figure 2). In a static field directly through the
surrogate, RB and GDL were found to be equivalent up to 4.5mm and 2.2mm water,
respectively. By comparing dose distributions in the TPS, DSC was found to be
0.989 and 0.997 for GDL and 0.897 and 0.954 for RB for a static field and a
VMAT plan, respectively. The RB and the GDL could be tracked in ranges [330˚,
60˚] and [330˚, 15˚], [-18˚, 18˚] and [-18°, +3˚], [-18˚, 18˚] and [-18˚, 11˚]
in yaw, pitch and roll, respectively.
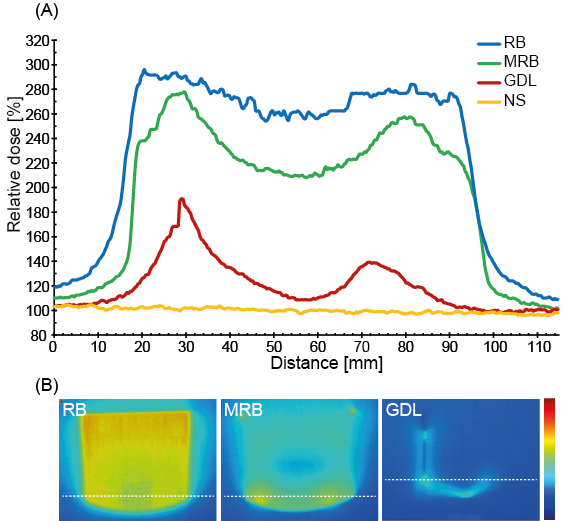
Figure 2: Film
measurements. (A) Profiles for GDL, RB and MRB at the entrance dose of the beam
compared to no surrogate (NS). (B) The position of the chosen profiles below
the three surrogates.
Conclusion
Gating Device L was found to have a
smaller dosimetric footprint than the Reflector Block. GDL had a lesser impact on
dose distributions compared to RB. While GDL was trackable in a smaller volume
of space, tracking was identical for GDL and RB in a clinically relevant range.
Gating Device L is therefore a promising alternative to Varian’s Reflector
Block.