Should we delineate brachial plexus in case of breast cancer hypofractionated radiotherapy?
PO-1562
Abstract
Should we delineate brachial plexus in case of breast cancer hypofractionated radiotherapy?
Authors: Fatma Dhouib1, Mariem Frikha2, Nejla Fourati2, Zied Fessi2, Leila Farhat2, Wafa Mnejja2, Jamel Daoud2
1Habib Bourguiba University Hospital, oncology-radiotherapy, Sfax, Tunisia; 2Habib Bourguiba University Hospital, Oncology-radiotherapy, Sfax, Tunisia
Show Affiliations
Hide Affiliations
Purpose or Objective
Hypofractionated radiotherapy (HRT) is becoming a
valid option in the treatment of breast cancer. However, data are missing
concerning the normal tissues dosimetric constraints. The purpose of
this study is to evaluate the cumulative doses in the brachial plexus during
hypofractionated locoregional irradiation for breast cancer with
a clinical toxicities correlation in order to
propose dosimetric constraints adapted to this
type of fractionation.
Material and Methods
This is a retrospective study analyzing the dosimetric
plans of 41 patients treated with adjuvant locoregional radiotherapy for
localized breast cancer between January and December 2020. The treatment plan
was carried out according to a three dimensional (3D) conformational technique.
The dose prescribed was 42.5 Gy in 16 fractions with a boost of 10 Gy in 4
fractions in the tumor bed in case of a conservative treatment (35%) and 40 Gy
in 15 fractions in case of a radical treatment (65%) at a rate of 5 fractions per
week. The delineation of the brachial plexus was performed according to the RTOG
guidelines and approved by two radiotherapy physicians. By analyzing the dose-volume
histogram, we retrospectively recorded the mean dose (Dmean), the maximum dose
(Dmax), the volume receiving more than: 32 Gy (V32) and 41 Gy (V41).These dosimetric constraint levels
were defined by calculating the biological equivalent dose. Clinical assessment
of radiation-induced brachial plexitis was performed at 12 months after the end
of radiotherapy using a questionnaire based on the modified LENTA-SOMA clinical
scales. Data analysis was performed by SPSS version 20.
Results
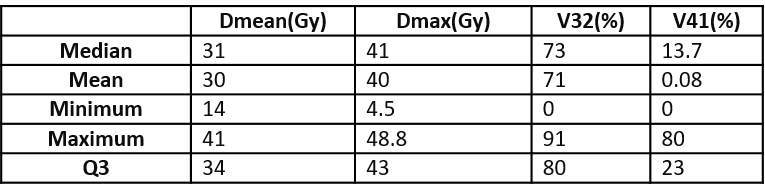
The median of the Dmean, Dmax, V32 and V41 were respectively of 31Gy [14-41], 41 Gy [4.5-41],
73% [0-91] and 0.08% [0-80]. The 3rd quartile (Q3) of Dmean, Dmax,
V32 and V41 were respectively of 34 Gy, 43 Gy, 80% and 23%.
The following table summarizes the
data of the cumulative doses in the brachial
plexus:
At twelve months after the end of the radiotherapy, fourteen patients
(34.14%) reported a radiation-induced brachial plexitis (grade 2 in 13 cases and
grade 3 in only one case). For all these patients, the Dmax was > 40 Gy and
the Dmean > 30 Gy.
Conclusion
The radiation-induced brachial plexitis is one of the most
underestimated complications in the locoregional treatment of localized breast
cancers. In the absence of radiation-induced plexitis prevention guidelines, we propose a systematic delineation of the brachial
plexus in case of locoregional breast cancer irradiation in order to minimize
as much as possible the cumulative doses at its level. The results of this
study show that these constraints could be reasonable to respect during
dosimetric optimization: Dmoy £30 Gy, Dmax £40 Gy and V41 £23%. However, these results should to be confirmed by
larger series.