Imaging dose distributions from CyberKnife robotic image guided radiotherapy
Panagiotis Archontakis,
Greece
PO-1536
Abstract
Imaging dose distributions from CyberKnife robotic image guided radiotherapy
Authors: Panagiotis Archontakis1, Panagiotis Papagiannis2, Ioannis Seimenis2, Evaggelos Pantelis2,3
1National and Kapodistrian University of Athens, Medical Physics Laboratory, Medical School, Athens, Greece; 2National and Kapodistrian University of Athens, Medical Physics Laboratory , Medical School, Athens, Greece; 3Iatropolis Clinic, Radiotherapy Department, Athens, Greece
Show Affiliations
Hide Affiliations
Purpose or Objective
In frameless radiosurgery,
in-room x-ray images and automated software routines are used to register the
planned dose distributions to the treated lesions with submillimeter accuracy. These
x-ray images are associated with an imaging dose to the patient. The purpose of
this work is to calculate the dose distributions from the image guidance x-ray based
system of the CyberKnife robotic radiosurgery system (AccurayTM
Inc., Sunnyvale, USA). Doses to the eye lenses and thyroid radiosensitive organs
are reported for typical intracranial treatments. In addition, beam hardening
filters of variable thickness were studied to minimize imaging dose.
Material and Methods
The CyberKnife system
employs two ceiling mounted x-ray kV tubes (40 - 150 kV) and two in-floor aSi
detectors. The imaging field is confined to (17x17) cm2 at isocenter
using trapezoidal collimators in order to cover the active surface of the detectors.
The image guidance system of the CyberKnife was modeled using the C++ class
library (egs++) of the EGSnrc Monte Carlo software package. The geometrical
characteristics of the developed model were based on the information shared by
the vendor. The total tube filtration was calculated based on Halve Value Layer
(HVL) measurements with the XR solid state detector (IBA Dosimetry, Germany)
positioned at the system isocenter. The x-ray spectrums used for sampling the
energy of the emitted photons were calculated using the SpekPy software
toolkit. Absorbed dose was calculated on digital patient models created using
corresponding Computed Tomography (CT) images and appropriate software tools of
the EGSnrc package. To minimize the imaging dose, additional simulations using Tin
beam hardening filters of variable thickness were studied.
Results
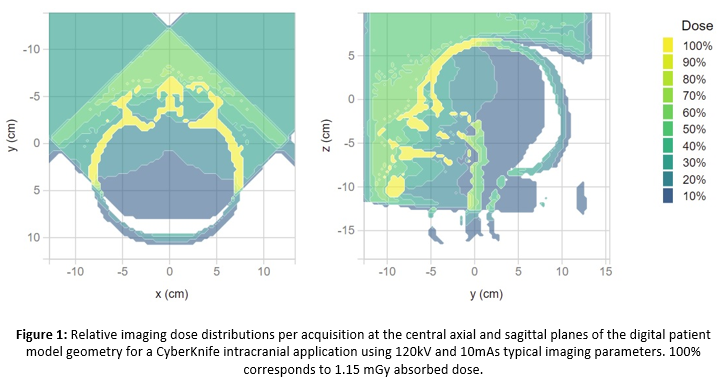
The absorbed imaging dose distributions
in an intracranial CyberKnife application is presented in Figure 1 using
nominal imaging parameters of 120 kVp and 10 mAs. The dose to the eye lenses from
both x-rays was found equal to 0.8 mGy
per acquisition. The dose to the thyroid which is outside the imaging field of
view for intracranial applications was found equal to 0.01 mGy per
acquisition. When Tin filter was used to
harden the imaging photon energy spectrum, the dose
was found to decrease reaching up to 20% for the lenses and for Tin filter
thickness of 1mm.
Conclusion
The absorbed dose to the
eye lenses from the image guidance in typical CyberKnife intracranial
applications (i.e., using 120 kVp and 10 mAs x-ray image acquisition
parameters) was found equal to 0.8 mGy
per acquisition. The presence of Tin filter was found to decrease the imaging
dose to the lenses by up to 20%. However, simulation findings should be
verified by corresponding measurements using optimized imaging parameters.