Using micro silica bead TLDs for 3D dosimetry in lung SABR treatments in a moving phantom
Wojciech Polak,
United Kingdom
PO-1535
Abstract
Using micro silica bead TLDs for 3D dosimetry in lung SABR treatments in a moving phantom
Authors: Wojciech Polak1, Shakardokht Jafari1, Antony Palmer2
1Portsmouth Hospital University NHS Trust,, Medical Physics, Portsmouth, United Kingdom; 2Portsmouth Hospital University NHS Trust, Medical Physics, Portsmouth, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To develop a verification technique for lung SABR treatment
delivery using silica TLD beads within a respiratory motion phantom that
provides a novel method for assessment
of 3D dose distribution inside and outside the target.
Silica bead TLD detectors (Trueinvivo Ltd, UK) with 1.1 mm
thickness and 1.6 mm diameter were characterised in previous studies for the MV
photon range used in radiotherapy plan deliveries [1,2]
Material and Methods
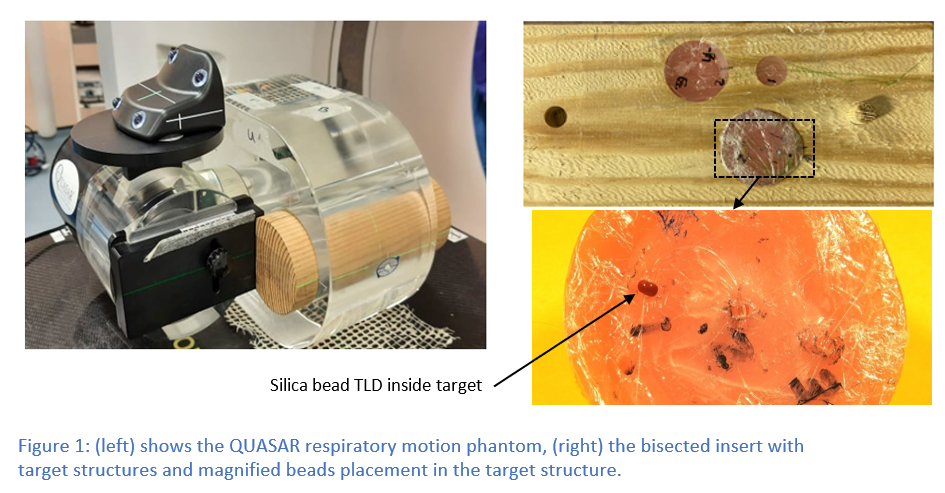
A respiratory
motion phantom (QUASAR™, Modus QA, US),
comprised a Perspex body section with custom-designed moving insert consisting
of a cedar wood cylinder to represent normal lung tissue, with three milled cavities
with diameters of 3, 2 and 1 cm filled with water-equivalent material infills (Fig.1).
Inside infills a range of ~1.7 mm cavities were drilled to accommodate TLDs (23
in total). The Phantom was scanned with 4DCT technique (4cm sup-inf amplitude
and 4 second period) with dummy beads located in cavities for accurate
localisation on the CT images
A SABR VMAT treatment
plan for largest infill (55Gy in 5#) was created in Pinnacle™ (TPS) on the
Average Intensity Phase (AIP) image following UK Consortium SABR guidelines. Plan
comprised of two 180 degrees arcs with 10MV FFF beam.
TLDs were calibrated
and individual bead sensitivities were established prior to experiment [1,2].
Two single fractions
and one full 5# of SABR treatment plan was delivered to the moving phantom with
separate sets of TLDs inserted in the prepared cavities for each delivery.
TLDs were readout
using a TOLEDO 654 Vinten TLD reader.
The treatment plan was transferred to each respiratory phase of 4DCT
dataset. TLDs locations were identified separately on each phase and TPS
calculated doses were noted for these points. Dose from each phase for the
particular TLD were added and compared with the measured doses
References:
- Jafari SM, et all: Radiation Physics and
Chemistry, 97, 95-101
- Jafari SM, et all: Physics in Medicine and
Biology, 59: 6875-6889
Results
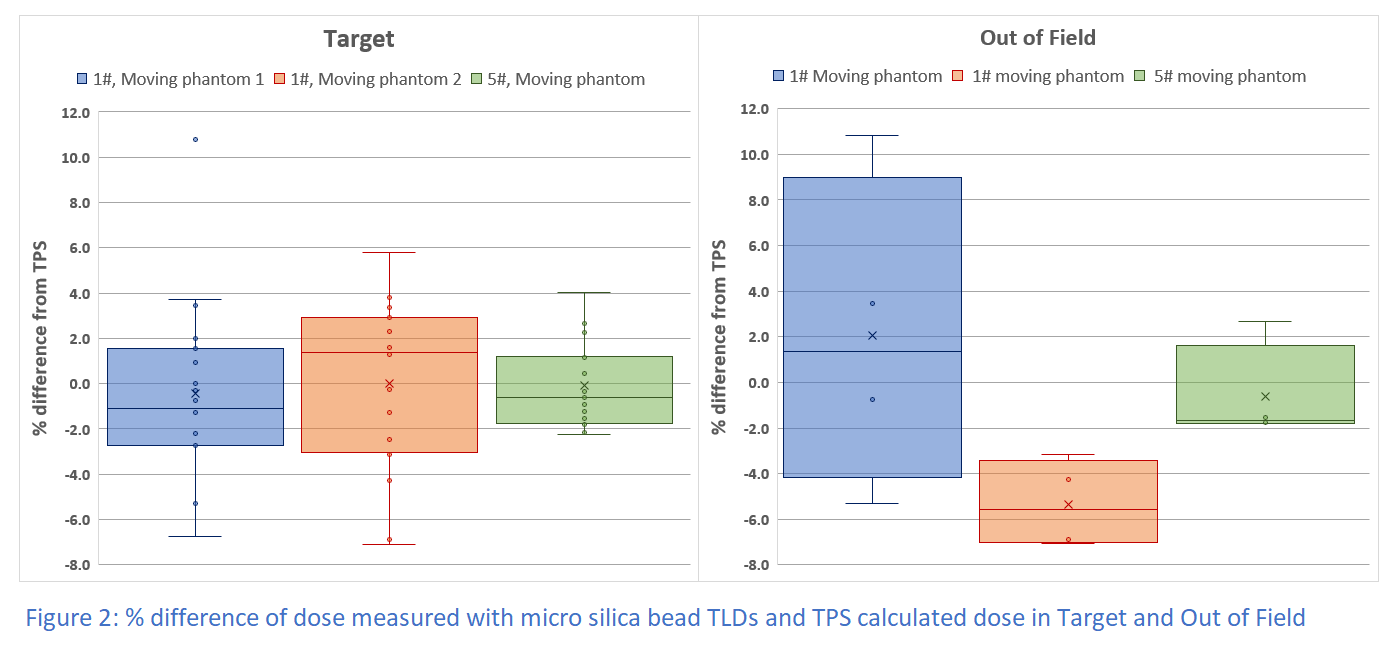
Comparison between measured dose and TPS dose is shown on Fig 2.
For points located in target measured dose difference ranged from -6.8% to +5.8%
for single fraction and from -2% to +4% for the 5# delivery. For points outside
target range was from -7.1% to +10.8% for single fractions and -1.8% to +2.7% for 5#
delivery.
Conclusion
A novel method of assessment of the lung SABR treatment delivery
was proposed. Accuracy of the dose delivery was assessed inside and outside of
the target. The 5# delivery produced best agreement between TPS calculated and TDLs measured
dose, both in target and out of field. The discrepancy between the predicted and
measured doses for single fraction deliveries are likely the result of the
interplay between the target and the delivery system respective motions. The
measurements results gave confidence in TPS beam model and confirmed viability
of using TLD beads to test the delivery.