Bone versus soft tissue setup in proton therapy for patients with oesophageal cancer
Muhammad Shamshad,
Austria
PO-1508
Abstract
Bone versus soft tissue setup in proton therapy for patients with oesophageal cancer
Authors: Muhammad Shamshad1,2, Ditte Sloth Møller2,3, Hanna Mortensen1, Mai Lykkegaard Ehmsen1, Maria Fuglsang Jensen1, Lone Hoffmann2,3
1Aarhus University Hospital, Danish Centre for Particle Therapy, Aarhus, Denmark; 2Aarhus University Hospital, Department of Medical Physics, Aarhus, Denmark; 3Faculty of Health Sciences, Aarhus University, Department of Clinical Medicine, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Proton therapy (PT)
may reduce dose to organs-at-risk compared to photon therapy (RT) which makes
PT favourable for oesophageal tumours where anatomical changes and respiratory
motion risk imposing target dose deterioration. The aim of this study was to
investigate the effect of patient (pt) positioning based on bone versus soft
tissue setup for PT in oesophageal cancer and the impact on plan adaptation in
preparation for the European randomized phase-III trial (PROTECT).
Material and Methods
This retrospective study included two consecutive patient cohorts (A and B)
with mid-thoracic, distal, or gastro-oesophageal junction (GEJ) cancer treated with RT.
Cohort A consisted of 26 pts who had a planning CT scan (pCT) and a surveillance
scan (sCT) acquired at fraction (fx) ten. Cohort B consisted of 180 pts who had
a pCT and were treated according to an adaptive strategy prompting a rescan CT
(sCT) in case of target under dosage due to anatomical changes observed on
daily CBCT. In cohort B 17 pts had sCT and were included in this study.
All CT scans were acquired as 10-phase 4DCT scans. The average scan created
from all phases was used for delineation and treatment planning. The iCTV (sum
of CTV in all respiratory phases) was used for optimization, total dose 50.4Gy
(RBE)/28 fx or 41.4Gy (RBE)/23 fx. Maximum dose to spinal cord was <45Gy
(RBE). A pencil beam scanning nominal plan was created using two posterior
beams with robust optimization using setup (5mm) and range (3.5%) errors. Robustness
towards respiration was evaluated by recalculating the plan on all respiratory
phases. Robustness towards setup (5mm) and range (3.5%) errors were evaluated.
For each patient, two rigid registrations were made between pCT and sCT: a
match on the vertebral column (4D bone match) and a match on the iCTV (4D soft
tissue). The treatment plan was recalculated on all phases of the delineated
sCT scan with each registration to evaluate the combined effect of respiration
and inter-fractional anatomical changes. Dose coverage of iCTV<97%
triggered adaptation. The statistical significance (p-value <0.05) of
iCTV dose coverage was assessed using the Wilcoxon signed-rank test.
Results
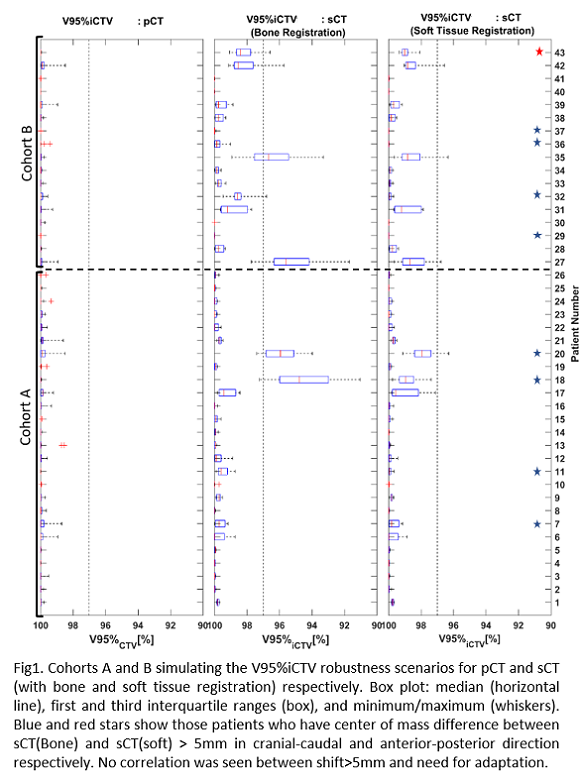
In all plans, V95%iCTV>99%
for the nominal plan and V95%iCTVtotal>97% for all respiratory and
robustness scenarios. Dose to the spinal cord was <45Gy (RBE) for all
plans at sCT. In cohort A, two (8%) and one (4%) pts needed adaptation
when bone and soft tissue registration was used. In cohort B selected
based on plan adaptation when treated with RT, five and three pts needed
adaptation for PT (see Fig 1). Dose coverage was significantly higher for soft
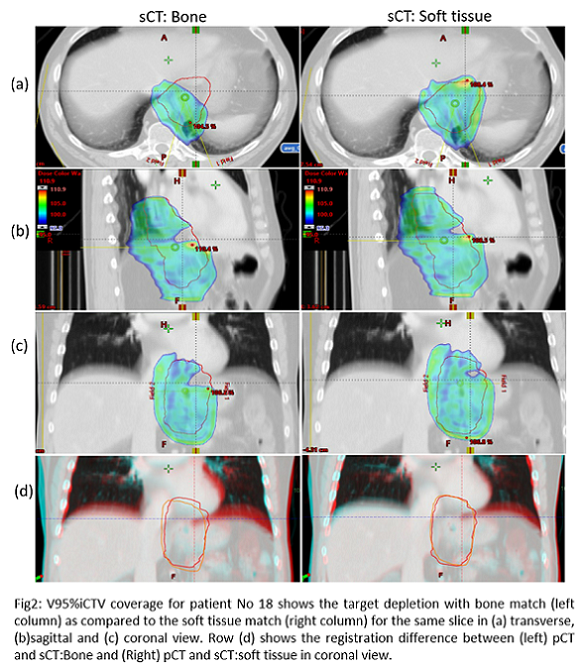
tissue setup. For patient 18 with a large shift between bones and tumour along
the cranio-caudal direction, target dose degradation was seen for the bone
match (Fig 2).
Conclusion
Anatomical changes during the treatment course led to larger target dose
deterioration and required more adaptation of proton plans having bone
registration than soft tissue match.