Comparing standard proton planning strategy for sinonasal cancer with pseudo-arc multifield approach
Raul Argota Perez,
Denmark
PO-1496
Abstract
Comparing standard proton planning strategy for sinonasal cancer with pseudo-arc multifield approach
Authors: Raul Argota Perez1,2, Ulrik Elstroem3, Kenneth Jensen3, Stine Korreman2,3,4
1Herlev Hospital, Department of Oncology, Herlev, Denmark; 2Aarhus University Hospital, Department of Oncology, Aarhus, Denmark; 3Aarhus University Hospital, Danish Center for Particle Therapy, Aarhus, Denmark; 4Aarhus University, Department of Clinical Medicine, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
A limited number of beam directions, often
non-coplanar, is commonly used when planning sinonasal cancer patients. While one
of the advantages of proton therapy is that there is no exit dose, there is
still entrance dose, and using just a few beam directions could result in a
high dose to the organs at risk (OARs) they are traversing. In this study, we
compared the commonly used planning strategy with a strategy using 11 coplanar
beams in a pseudo-arc setup, and evaluated and compared the effect in the dose
to the OARs.
Material and Methods
Retrospective proton (IMPT) plans were made for 24
sinonasal cancer patients in Eclipse v15.6. Dose was 66-68Gy/60-66Gy for
primary/postoperative radiotherapy. The strategies evaluated were: S1, which
consisted of 3-4 beams angles; and S2, 11 beams angles spaced 20 degrees through
the front (avoiding the nose). A range shifter of 5 cm was used for S1 for
beams where the water equivalent distance between skin surface and target in
beams-eye-view was <4cm. For S2 the range shifter was avoided if acceptable
target coverage could be achieved without, but if needed was used for all
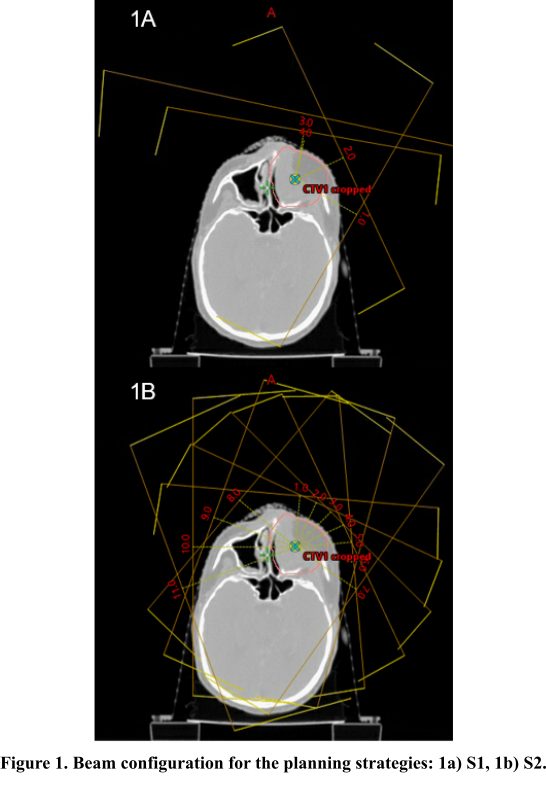
fields. Beam configurations are shown in
Figure 1. All plans were optimized with robust optimization (RO) and multifield
optimization. For RO setup uncertainty of ± 2mm in all cardinal directions and
± 3.5% range uncertainty were used (14 scenarios in total). For robustness
evaluation (RE), the same parameters were used. Dose to OARs was evaluated and
compared between the strategies.
Results
For 9/24 patients, it was necessary to use range
shifter for S2, in order to reach acceptable coverage for all RE scenarios.
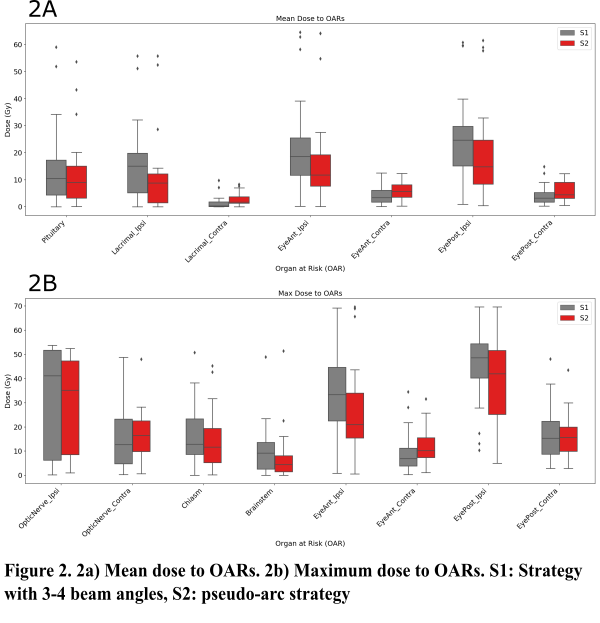
Mean dose to OARs in the ipsilateral side was lower
for S2 than for S1 (Figure 2a). For example, mean doses to the ipsilateral
posterior eye were 24.7Gy/14.8G for S1/S2 (population median). Organs farther
away from the target or in the contralateral side, received a lower dose with
S1 compared to S2. For example, mean doses to the contralateral posterior eye
were 3.3Gy/4.5Gy for S1/S2 (population median).
The same tendency was observed for maximum doses
(Figure 2b). Maximum doses to the ipsilateral anterior eye were 37.6Gy/21.0Gy for
S1/S2 (population median), while maximum doses to the contralateral optic nerve
were 12.7Gy/16.5Gy for S1/S2 (population median).
Even when range
shifter (RS) had to be used in S2, there was still a benefit for some
ipsilateral organs – see maximum dose (population median) in table below.
| Ipsi optic nerve | Ipsi optic nerve | Ipsi anterior eye | Ipsi anterior eye |
| S1 | S2 | S1 | S2 |
Pts with RS in S2
| 3.7 | 5.8 | 38.1 | 33.3 |
Pts without RS in S2
| 48.8 | 41.9 | 33.4 | 20.1 |
Conclusion
OARs in the proximity of the target benefited from
using multiple beams in a pseudo-arc, but this resulted in an increased low
dose for OARs farther away from the target. The use of range shifter gave a
lower benefit of using multiple beams. An evaluation of the effect of the
day-to-day anatomical variations during the treatment of the different planning
strategies is presently being performed.