Long-term survival after radiotherapy in oligoprogressive patients during checkpoint inhibition
Pim Damen,
The Netherlands
PO-1451
Abstract
Long-term survival after radiotherapy in oligoprogressive patients during checkpoint inhibition
Authors: Pim Damen1, Karijn Suijkerbuijk2, Sherif El Sharouni1, Anne van Lindert3, Wietse Eppinga1, Joost Verhoeff1
1UMC Utrecht, Radiation Oncology, Utrecht, The Netherlands; 2UMC Utrecht, Medical Oncology, Utrecht, The Netherlands; 3UMC Utrecht, Pulmonology, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Recent studies described safety and clinical utility of combined anti-programmed cell death protein-1 (anti-PD1) checkpoint inhibition with radiotherapy. However, long-term follow-up data is lacking. Abscopal effects – radiotherapy inducing clinically meaningful distant responses in unirradiated sites - have been hypothesized, though clinical proof is still scarce.
Material and Methods
We retrospectively analysed long-term efficacy and toxicity of combined (stereotactic body) radiotherapy and anti-PD1 in consecutive oligoprogressive stage IV melanoma and non-small cell lung cancer (NSCLC) patients who were irradiated for 1 to 3 progressive metastases during anti-PD1 in our institute between January 2017 and January 2019 and verified one-dimensional RECIST measurements by volumetric assessments.
Results
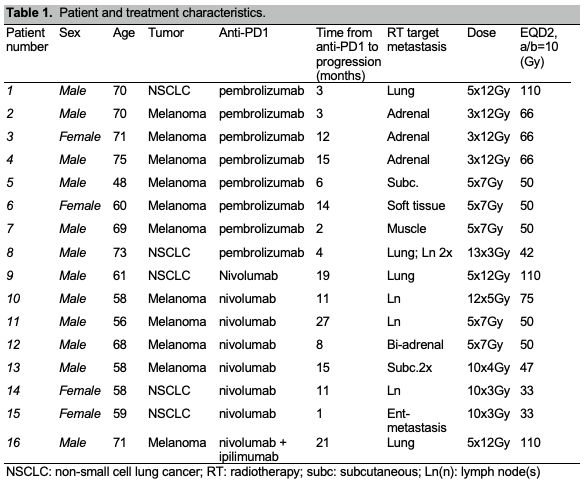
In total 361 stage IV melanoma and NSCLC patients were treated with checkpoint inhibitors in this period. Only 16 of these patients (11 melanoma and 5 NSCLC) were treated with extra-cranial (stereotactic body) radiotherapy for local oligoprogression during checkpoint inhibition and were included in this series. Patient and treatment characteristics are shown in Table 1. Radiotherapy was applied after a median of 11 months (range 1-30 months) from start of anti-PD1 treatment. No increased risk of adverse events for the combined treatments was observed. Sixty-nine percent of patients were alive after a median follow-up of 4.5 years since start of anti-PD1. Seven of 16 patients had stable disease after a median follow-up of 3.5 years after radiotherapy. Abscopal effects were suspected in 3 out of 16 patients. However, if volumetric assessment was used, 2 of these patients already had tumor shrinkage prior to radiotherapy, not detected by one-dimensional measurements.
Conclusion
Our series show that (stereotactic body) radiotherapy for oligoprogressive disease during PD1-inhibition can induce long-term disease control and overall survival. Although abscopal effects were suspected in 3 patients, they were not confirmed with volumetric assessment in 2 patients. The discrepancy found between one-dimensional and volumetric response assessment argues for including volumetric assessment in further studies.