Characterising anatomical changes of head and neck cancer patients during radiotherapy treatment
Poppy Nikou,
United Kingdom
PO-1492
Abstract
Characterising anatomical changes of head and neck cancer patients during radiotherapy treatment
Authors: Poppy Nikou1, Andrew Nisbet1, Anna Thompson2, Sarah Gulliford3, Jamie McClelland1
1University College London, Department of Medical Physics, London, United Kingdom; 2University College London Hospital, Department of Radiotherapy , London, United Kingdom; 3University College London Hospital, University College London, Department of Radiotherapy Physics, Department of Medical Physics, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Inter-fractional anatomical changes can lead to
uncertainties in the delivered dose distribution. To address this, there is an
interest in modelling the anatomical changes which occur over the course of
treatment. To inform the choice and complexity of the model, this project aimed
to identify and quantify the inter-fractional anatomical changes of head and
neck (H&N) cancer patients.
Material and Methods
A cohort of
20 H&N cancer patients treated with IMRT were studied. Each patient
had a planning CT (pCT), a rescan CT (rCT) and a series of CBCTs (4-10). A
diffeomorphic deformable image registration aligned each CBCT to the pCT. The
transformation was used to warp the pCT structures to each CBCT. To test the
accuracy of the DIR, two independent geometric validation tests were performed.
The warped contours were compared to (1) the rCT contours, (2) contours which
were manually delineated on CBCTs. A longitudinal volumetric analysis was
performed on each structure. A leave one out cross validation analysis determined
the best function to parameterise the changes.
Results
The
geometric validation tests showed a good correspondence between the warped and
ground truth contours. The average difference in distance was found to be on
the order of the thickness of a CT slice (mm). A quadratic function was calculated
as the best fit for the changes in parotid gland volume. In comparison, all
other structures were best parameterised with a linear fit (high and low dose CTV,
body). Structures can therefore be differentiated depending on their rate of
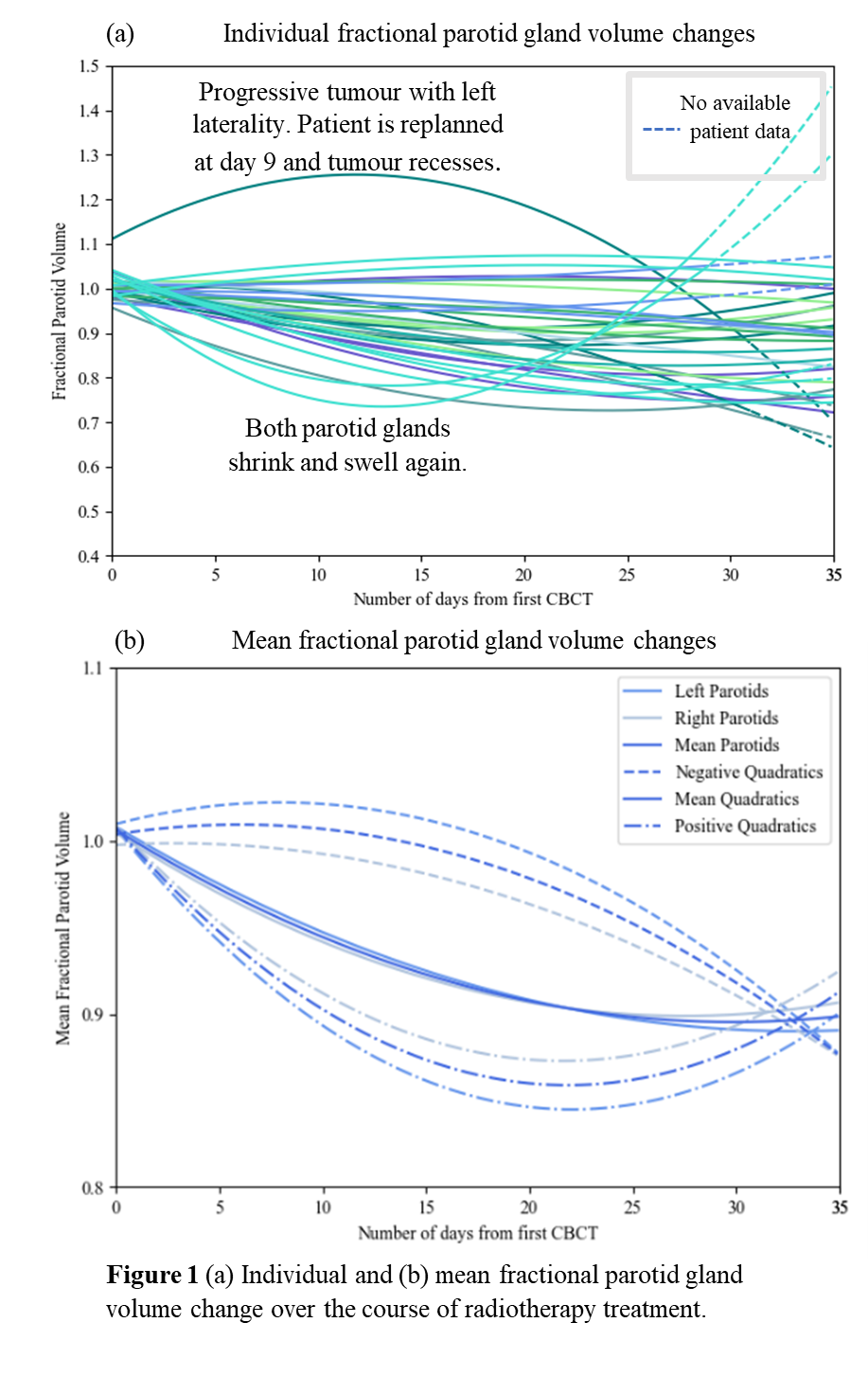
volume change during treatment: constant or variable. Figure 1 shows the (a) individual
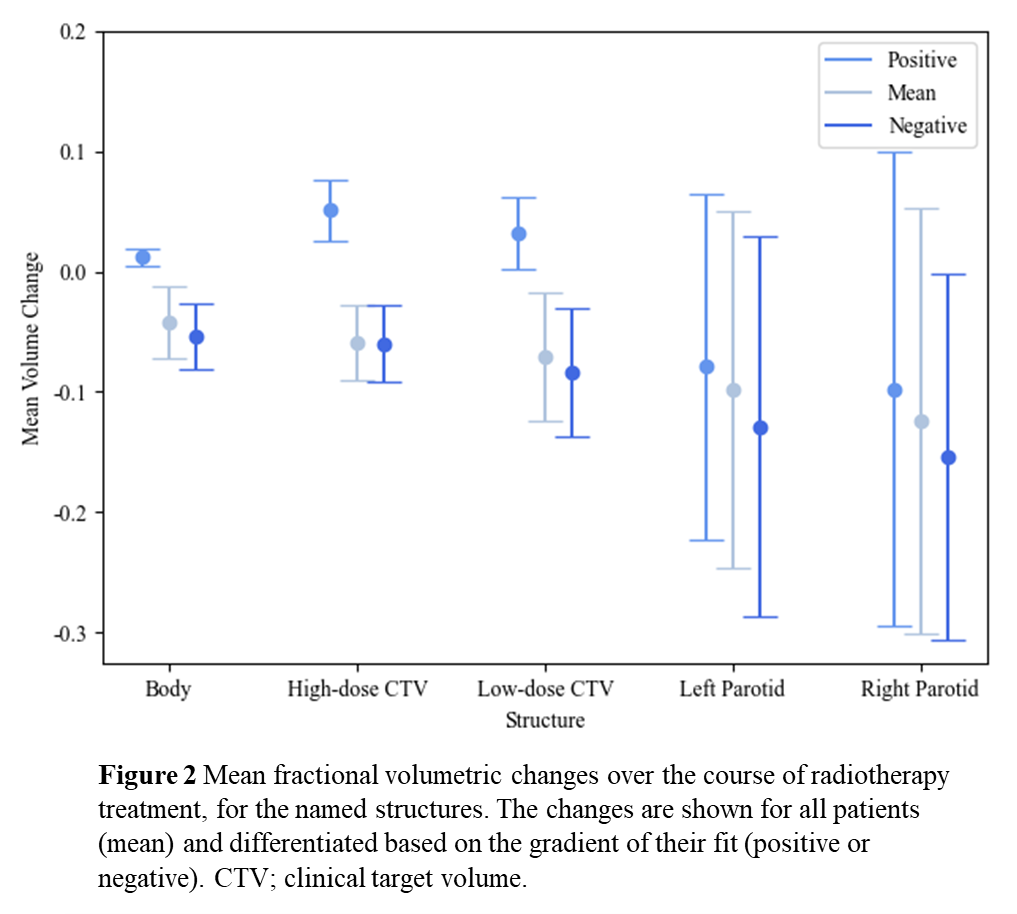
and (b) mean fractional parotid gland volume changes. Figure 2 shows the
average volume changes at the end of treatment (day 35), compared to the start
of treatment, for all structures. Both figures indicate a broad patient
variability within the population, especially in the final parotid gland
volumes.
Conclusion
H&N
cancer patients are subject to large anatomical changes during fractionated
radiotherapy. For most patient structures the volume decreases during treatment.
The rate of volume change over treatment however, is structure and patient
dependent. Therefore, complex models are needed to account for the patient specific
variability.