Residual setup error of the pelvic lymph nodes after prostate based IGRT of prostate cancer patients
PO-1489
Abstract
Residual setup error of the pelvic lymph nodes after prostate based IGRT of prostate cancer patients
Authors: Emil Fredén1, Johan Knutsson1, Gracinda Johansson1
1Södersjukhuset, Department of Oncology, Stockholm, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
In the RT
of prostate cancer (PCa), simultaneous irradiation of the prostate and pelvic
lymph nodes (pLN) requires application of separate CTV-to-PTV margins, since the
two target volumes move independently of each other. IGRT protocols aiming to
correct for inter-fraction prostate displacements inevitably lead to a residual
setup error (RSE) of the pLN. This error must be quantified and included in the
calculation of pLN margins. In the present study, we quantified the pLN RSE resulting
from a prostate based IGRT protocol and calculated the corresponding pLN margins.
Material and Methods
580
treatment fractions from 21 PCa patients that received simultaneous irradiation
of the prostate and pLN were included. These patients were initially positioned
with the Catalyst surface scanning system (C-RAD, Uppsala, Sweden). Thereafter,
a CBCT was acquired to derive the couch translations necessary to align the
prostate in accordance with the planning CT (pCT) based on a registration of gold
markers. The online registrations were performed in the XVI system (Elekta AB,
Stockholm, Sweden). To estimate the pLN RSE, we calculated the difference
between these couch translations and translations derived from an offline grayscale
registration performed in Mosaiq (Elekta AB, Stockholm, Sweden). For the
grayscale registrations, bony anatomy up to the fifth lumbar vertebra were
included. For each grayscale registration, a visual assessment was performed to
verify that the bony anatomy had been correctly aligned with the pCT. Rotations
derived from the grayscale registration were excluded but were manually
converted into translations if deemed necessary after visual assessment. The RSE
in pLN position was estimated separately in each of the three orthogonal
directions. The population systematic uncertainty and random uncertainty of the differences in each direction were
calculated and used as input to anisotropic pLN margin calculations, for which
we used van Herk’s margin formula. In addition to the pLN RSE, we considered several
uncertainty components as either estimated from routine QA measurements, or based
on values from the literature.
Results
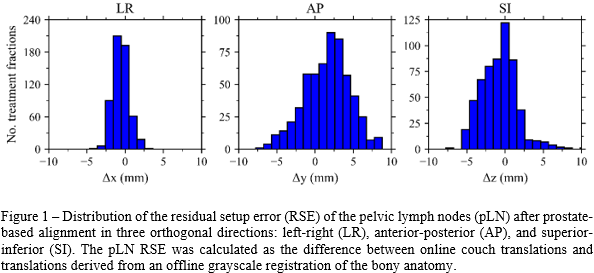
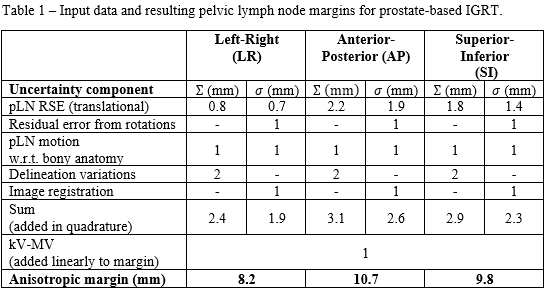
The
resulting distributions of the pLN RSE are shown in Figure 1. The systematic-
and random uncertainty of this data set was used together with the additional uncertainty
components to calculate anisotropic pLN margins, see Table 1. The resulting
margins were 8.2 mm, 10.7 mm, and 9.8 mm in the left-right (LR),
anterior-posterior (AP), and superior-inferior (SI) direction, respectively.
Conclusion
Our current
isotropic pLN margins of 13 mm for prostate based IGRT can safely be reduced. Margin
reduction allows for reduction of dose to organs at risk but can also enable target dose
escalation. However, margin reduction must be based on careful consideration of
all uncertainties in the planning- and treatment process. Each clinic should therefore
derive their own treatment margins based on locally estimated uncertainties.