A predictive model to quantify the dosimetric impact of inter-fraction variability in breast cancer
PO-1483
Abstract
A predictive model to quantify the dosimetric impact of inter-fraction variability in breast cancer
Authors: Martina Iezzi1, Davide Cusumano2, Danila Piccari3, Sebastiano Menna2, Francesco Catucci3, Andrea D'Aviero4, Alessia Re4, Carmela Di Dio4, Flaviovincenzo Quaranta4, Althea Boschetti4, Marco Marras3, Domenico Piro3, Claudio Votta3, Eleonora Sanna3, Chiara Flore3, Gian Carlo Mattiucci2, Vincenzo Valentini5
1Institute of Radiology, Università Cattolica del Sacro Cuore, Department of Radiological and Hematological Sciences, Rome, Italy; 2Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Departemet of Radiation Oncology, Rome, Italy; 3Mater Olbia Hospital, Departemet of Radiation Oncology, Olbia, Italy; 4Mater Olbia Hospital, Department of Radiation Oncology, Olbia, Italy; 5Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Department of Radiation Oncology, Rome, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Breast cancer is one of the anatomical sites where standard radiotherapy (RT)
has today a very established role, so the benefits brought by the introduction
of any new variation has to be carefully assessed.
As a discipline in its infancy, online adaptive RT (ART) needs new
ontologies and ad hoc criteria to evaluate the appropriateness of its use in
clinical practice. In this experience we propose a predictive model able to
quantify the dosimetric impact due to daily inter-fraction variability in a standard
RT breast treatment, to early identify the treatment fractions where patients
might benefit of an online ART approach.
Material and Methods
The study was focused on right breast patients treated
using standard adjuvant RT on an Artificial Intelligence (AI)-based linear
accelerator (Ethos, Varian Medical System).
Patients
were treated with daily CBCT images and without online adaptation, prescribing
40.05 Gy in 15 fractions, with a IMRT technique consisting in four tangential
beams.
ESTRO
guidelines were followed for the delineation on planning CT (pCT) of organs at
risk (OARs) and target volumes: CTV was defined as entire mammary gland, PTV as
CTV+5 mm in LR and 7 mm in AP and CC direction, with 5 mm crop margin from the
body. For each patient, all the CBCT images were rigidly aligned to pCT,
excluding rotational shifts according to Ethos workflow.
CTV
and PTV were manually re-contoured on daily CBCT images, and the original treatment
plan was recalculated. Various radiological parameters were measured on CBCT
images, with the aim of quantifying inter-fraction variability present in each
RT fraction after couch shifts compensation. The absolute difference in terms
of body between daily CBCT and pCT was calculated along each beam axes, considering
the isocentre plan as reference plan. The variation of these parameters was
correlated with the variation of V95% of PTV (ΔV95%) using the Wilcoxon Mann
Whitney test. Fractions where ΔV95>2% were considered as adverse events. A
linear regression model was calculated considering the most significant parameter
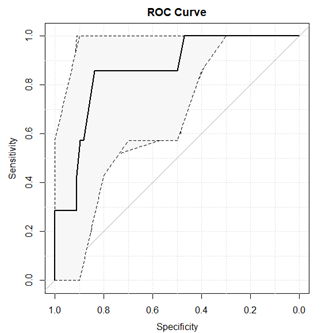
and its performance were quantified in terms of Receiver Operating
Characteristic (ROC) curve
Results
A total of 75 fractions on 5 patients were analysed. The body variation along
the beam axis with the highest MU was identified as best predictor (p=0.002).
The predictive model elaborated showed an area under under ROC curve of 0.86 (0.82-0.99
as 95% CI) with a sensitivity of 85.7% and a specificity of 83.8% at the best
threshold which was equal to 3 mm (Figure 1).
Conclusion
A novel
strategy to identify treatment fractions which may benefit of online ART was
proposed. After image alignment, the measure of body difference between daily CBCT
and pCT can be considered as an indirect estimator of V95% PTV variation: a
difference larger than 3 mm will results in a V95% decreased of more than 2%. A
larger number of observations is needed to confirm the results of this
hypothesis generating study.