Radiological measurements to predict dose variation due to inter-fraction variability in H&N
PO-1481
Abstract
Radiological measurements to predict dose variation due to inter-fraction variability in H&N
Authors: Francesco Catucci1, Davide Cusumano2, Sebastiano Menna2, Andrea D'Aviero1, Carmela Di Dio1, Alessia Re1, Martina Iezzi3, Danila Piccari1, Flaviovincenzo Quaranta1, Althea Boschetti1, Marco Marras1, Domenico Piro1, Claudio Votta1, Eleonora Sanna1, Chiara Flore1, Gian Carlo Mattiucci4, Vincenzo Valentini4
1Mater Olbia Hospital, Radiation Oncology, Olbia, Italy; 2Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Department of Radiation Oncology, Rome, Italy; 3Università Cattolica del Sacro Cuore, Radiation Oncology, Roma, Italy; 4Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Radiation Oncology, Roma, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Several experiences
have demonstrated the benefit of adaptive radiotherapy (ART) in patients
affected by head and neck squamous cell carcinoma (HNSCC), both considering
offline and online strategies. As a new discipline, online ART requires new indicators to quantify the
impact of inter-fraction variations on dose distribution, thus allowing identification
of the optimal time to switch towards online ART approaches. In this
experience, a predictive model was proposed to early identify treatment
fractions where unacceptable dose variations may be present
Material and Methods
Patients affected by HNSCC were treated using an Artificial
Intelligence-based linac (Varian Ethos) with 12 IMRT beams, acquiring a daily
positioning CBCT image without online adaptation, prescribing 70 Gy in 35 fractions
with normalisation at median dose.
For each patient, all CBCT
images acquired for patient positioning were rigidly matched to the planning CT
(pCT), excluding rotational shifts according to Ethos clinical workflow. Daily
CBCT images were automatically recontoured and treatment plan were recalculated
on the corresponding synthetic CT. The variation of V95% of PTV1 and max dose
of spinal cord from the original values reported on pCT were collected along the
treatment: fractions where PTV V95% decreased of 3% and spinal cord Dmax
increased of 5% were considered as needed of ART.
The following radiological
parameters were measured on each daily CBCT aligned with pCT to quantify the
inter-fraction variability present in each RT fraction once compensated for
couch shifts: the absolute body variation along AP and LR directions measured
in proximity of the plans passing through different vertebrae (C1, C2, C3 C4)
and the corresponding discs (C1-C2, C2-C3, C3-C4).
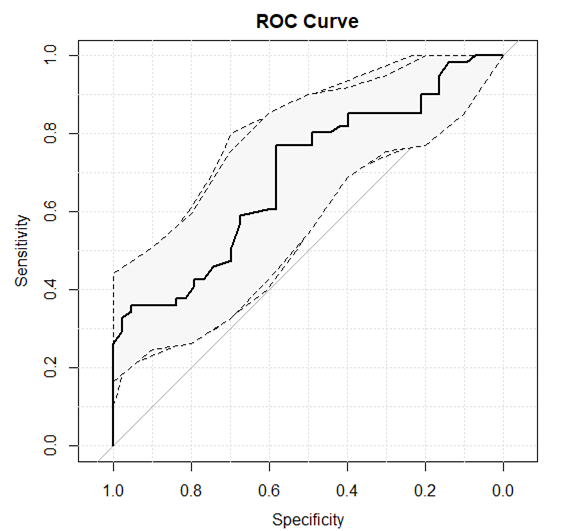
The correlation between such
parameters and the fractions needed of adaptation was investigated using the Wilcoxon
Mann Whitney test. A logistic regression was calculated considering the most
significant radiological parameter and the predictive performance were
quantified considering the Receiver Operating Characteristic (ROC) curve.
Results
On the basis of the
predefined criteria, 61/104 fractions
analysed required online adaptation. At
the univariate analysis the most
significant parameter was the body variation along the AP direction measured
through the C3-C4 disc (p=0.0002). The developed predictive model (ROC curve in
fig.1) showed an AUC of 0.69 (0.59-0.79 as 95% CI) with sensitivity of 77.1% and
specificity of 58.2% at the best threshold, which was 3 mm
Conclusion
A new metric to define the need of online ART was
proposed based on body variation measured along the AP direction through the
C3-C4 disc: if such value results > 3 mm the treatment fraction has to be
considered needed of ART (92% of probability of not meeting the tolerance
criteria). If confirmed on larger cohorts, this strategy could be used as
indirect metric to establish the optimal timing of replanning also in center
not equipped with online ART technologies