SGRT setup patient accuracy in breast cancer patients compared to two different IGRT workflows
Cristina Anson Marcos,
Spain
PO-1479
Abstract
SGRT setup patient accuracy in breast cancer patients compared to two different IGRT workflows
Authors: Cristina Anson1, Nuria Jornet1, Noé Ventosa2, Sonia Bermejo2, Jaime Pérez-Alija1, Pedro Gallego1, Artur Latorre-Musoll1, Nagore García1, Helena Vivancos1, Marta Barceló1, Agustín Ruiz1, Fátima Leo1, Pablo Carrasco1
1Hospital de la Santa Creu i Sant Pau, Medical Physics, Barcelona, Spain; 2Hospital de la Santa Creu i Sant Pau, Radiation Oncology, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Surface guided radiotherapy (SGRT) is reported to
improve patient setup for whole‐breast radiotherapy. The purpose of this study
is to evaluate the patient SGRT accuracy for pre-imaging setup considering two
different IGRT workflows: orthogonal kV-MV images and CBCT guidance.
Material and Methods
Patient setup accuracy during the first treatment
session of 31 breast cancer patients was retrospectively evaluated. The
workflow was performed in a TrueBeam unit and the optical SGRT system Align-RT
(Vision-RT) as follows:
- First, patients were positioned by aligning
tattoos to the room lasers and TPS isocentre shifts were applied to the couch.
After this, patient arms and breast surface were matched to the simulation
position with the aid of Vision RT postural video license and a ROI including the
breast. From this, system delta couch shifts were performed only for the three
directions: vertical, lateral and longitudinal, and recorded as ‘SGRT’ deviation.
- Orthogonal kV-MV images guidance were acquired. The
register was done to bony structures (rib bone and sternum). Differences
between initial (pre-imaging) and treatment couch positions were then recorded
as ‘KV-MV’ deviation.
- Immediately after, a CBCT was performed and an
automatic image registration to the PTV structure was done. Differences between
initial (pre-imaging) and treatment couch positions were then recorded as
‘CBCT’ deviation.
If the deviations either with kV-MV or CBCT images were within 0.5 cm
tolerance, no table shift was applied.
Results
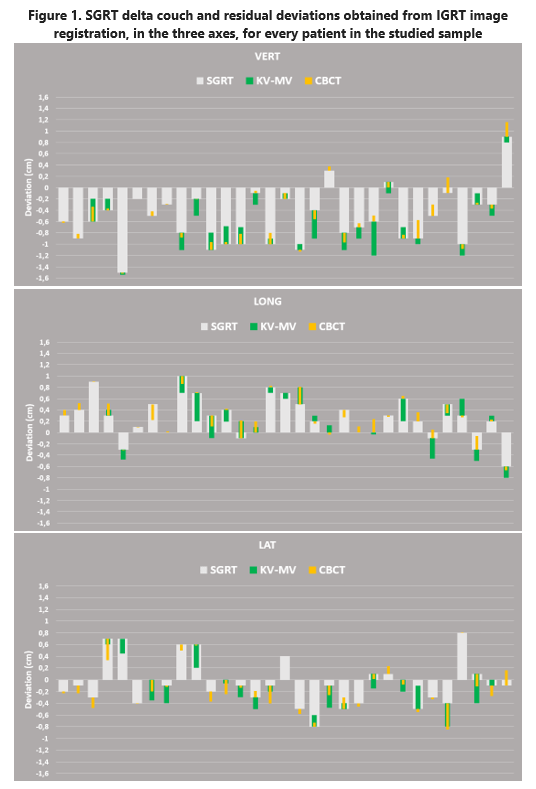
Figure 1 shows the couch shifts applied from SGRT system. From these
values, the IGRT image registration deviations are displayed.
Except for
one patient, IGRT deviation values were within tolerances, so no additional
couch shifts were performed after SGRT setup. The exception was for KV-MV with
0.6 cm deviation in vertical axis, meanwhile the CBCT deviation was 0.2 cm.
For most
patients the deviation obtained from CBCT registration was smaller (0.1±0.1,
0.0±0.1 and -0.1±0.2 in cm for vert, long and lat axes respectively) than the
one obtained with orthogonal planar kV-MV imaging (0.0±0.2, -0.1±0.2, -0.1±0.2 cm vert, long, lat respectively).
Even though the CBCT imaging was performed after kV-MV imaging and the patient
could have moved. The
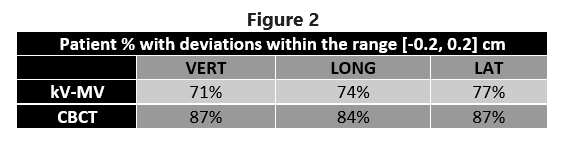
percentages of patients with imaging derived differences within the interval [-0.2,
0.2] cm are shown in Figure 2.
Conclusion
Optical 3D surface imaging for breast cancer patient
setup positioning showed an excellent agreement with CBCT images (less than 2
mm residual for most patients) and better than for kV-MV.
Positioning breast patients daily with SGRT could lead
to a reduction to CTV to PTV margins without a cost of imaging dose linked to
daily CBCT imaging.