Evaluation of two generic algorithms for CBCT based dose calculation
PO-1477
Abstract
Evaluation of two generic algorithms for CBCT based dose calculation
Authors: Rune Thing1, Rasmus Nilsson2, Sebastian Andersson2, Martin Berg1, Mikkel Lund1
1Vejle Hospital, University Hospital of Southern Denmark, Dept. of Oncology, Vejle, Denmark; 2RaySearch Laboratories, Research, Stockholm, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
Two
algorithms for post-processing of uncalibrated CBCT images were evaluated for
all patient groups treated with curative intent at Vejle Hospital, with
emphasis on dosimetric accuracy and applicability for offline treatment
adaptation.
Material and Methods
CT and CBCT
images of 60 patients were identified. Patients were distributed with 10
breast, 10 lung, 10 prostate, and 10 anal or rectal cancer patients with
original treatment plans optimized on CT images, and additionally 10 prostate
and 10 anal or rectal cancer patients with treatment plans optimized on
synthetic MR-derived (MRCAT) images. Treatment planning and CBCT based
recalculation was performed in RayStation (research build v10.1.110.51).
“Clinical CBCT” (clinCBCT) dose was calculated on CBCT images acquired on the
Elekta XVI system for IGRT, after assignment of standardized bulk densities.
Additionally, two synthetic CBCTs were created per patient. A “corrected CBCT”
(corrCBCT), calculated from deformable image registration (DIR) and 2D joint
histogram analysis, and a “virtual CT” (vCT) created by DIR of the original
planning CT to the clinCBCT image while correcting for local variations such as
bowel gas etc.
Dosimetric accuracy was evaluated through gamma pass rate analysis with 2%/2mm
and 1%/1mm criteria, as well as by evaluating D2% to organs at risk (OAR) and
D50% to delineated target structures (propagated to the CBCT images using DIR).
The reference image for comparison was chosen as a reference CT (refCT) as
close in time as possible (same day CT for 21 patients who were rescanned during
the treatment course, and planning CT vs. first fraction CBCT for the remaining
39 patients), with additional DIR performed to minimize anatomical variations.
Results
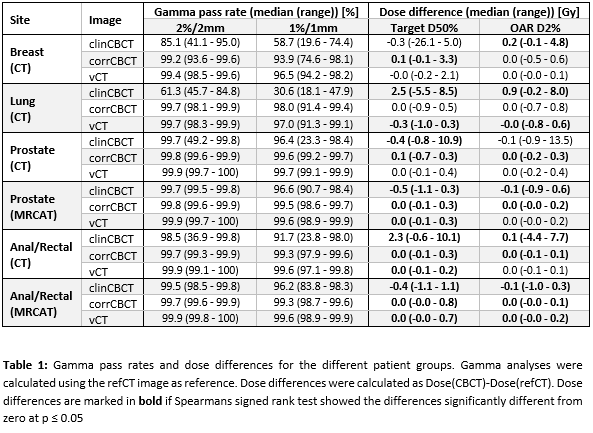
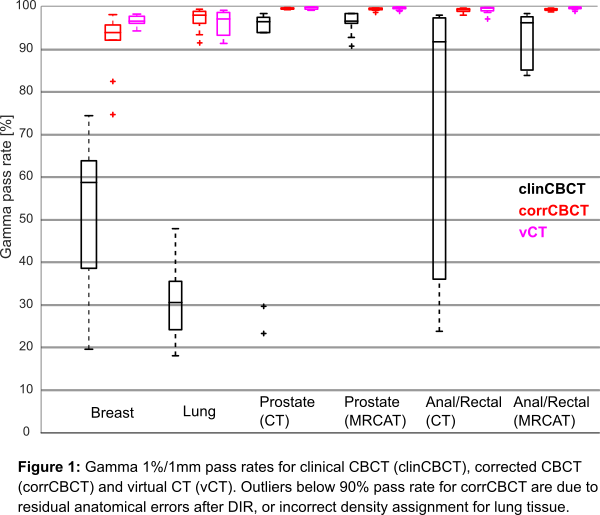
Gamma pass
rates and DVH metrics are shown in Table 1. For the clinCBCT images, Gamma
2%/2mm pass rates as low as 37% are observed, while the corrCBCT and vCT
present pass rates no less than 93.6% and 98.3%, respectively. At the 1%/1mm
criterion (Figure 1), the clinCBCT median pass rate for the lung patients is as
low as 30.6% (range 18.1-47.9%), while corrCBCT images pass at 98% of points in
median (range 91.4-99.4%), and the vCT images pass at 97% of points (median,
range 91.3-99.1%).
DVH metrics
for the clinCBCT images showed a very wide range in difference for target D50%,
from -26.1Gy for a breast patient to +10.9Gy for a CT-based prostate patient. OAR
D2% ranged from -4.4Gy for an anal/rectal patient, up to +13.5Gy for a CT-based
prostate patient. For the corrCBCT and vCT images, all variations were less
than ±1Gy (targets and OAR). None of the CBCT based dose distributions were
consistently unskewed in Spearmans signed rank test.
Conclusion
corrCBCT
and vCT images provide accurate dose calculations, highly suitable to assist
any strategy for offline dose-based adaptive radiotherapy, without needs for
individual CBCT calibration or limitations to certain anatomical sites, CBCT acquisition protocols, or planning CT modality.