assessment of online adaptive MR-Guided prostate SBRT with integrated boost to dominant lesion
PO-1399
Abstract
assessment of online adaptive MR-Guided prostate SBRT with integrated boost to dominant lesion
Authors: Kyle Padgett1, Jonathan Cabrera2, William Jin1, Hayden Guerrero1, Matthew Abramowitz1, Matthew Studenski1, Nesrin Dogan1
1University of Miami, Radiation Oncology, Miami, USA; 2University of Miami, Biomedical Engineering, Miami, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Online
Adaptive Radiotherapy (ART) with daily MR imaging has the potential to improve
dosimetric accuracy by accounting for anatomical changes during radiotherapy. Existing
daily ART prostate studies have diverse conclusions, but lack information
regarding integrated boosts to the dominant intraprostatic lesion, which has
shown an increase in biochemical disease-free survival. The purpose of this
study is to determine the potential dosimetric gain of daily ART to the dominant
lesion and other targets as well as potential benefits to the OARs.
Material and Methods
Five patients with prostate
cancer treated with MR-Guided SBRT are included. Prescription to the planning
target volume (PTV) was 36.25Gy in 5 fractions and the prescription to the intraprostatic
boost (GTV) ranged between 40-45Gy. The normalization for the PTV ranged from
90-95% coverage at the Rx dose and >90% coverage for the GTV. All patients underwent a planning MRI and planning CT as
well as daily setup MRIs prior to each fraction. The organs-at-risk (OARs)
included bladder, anorectum, bowel, femoral heads, and penile bulb. The CTV encompassed
the prostate and proximal seminal vesicles, the PTV is an expansion of the CTV
by 4-5mm in all directions except 3mm posteriorly. The GTV was defined using
mpMRI and confirmed by MRI guided TRUS biopsy (no margin). The initial
treatment plan was generated using step-and-shoot IMRT. The electron density
map and contours from the planning MR were propagated to the daily setup MRI
using deformable image registration and the contours were then edited. Each
adapted fraction was obtained by re-optimizing based on the contours on daily
setup MRI. Non-adaptive fractions were simulated by re-calculating the dose on each
daily setup MRI. Non-adaptive and adaptive fractions were compared using target
coverage and OAR dose-volume metrics.
Results
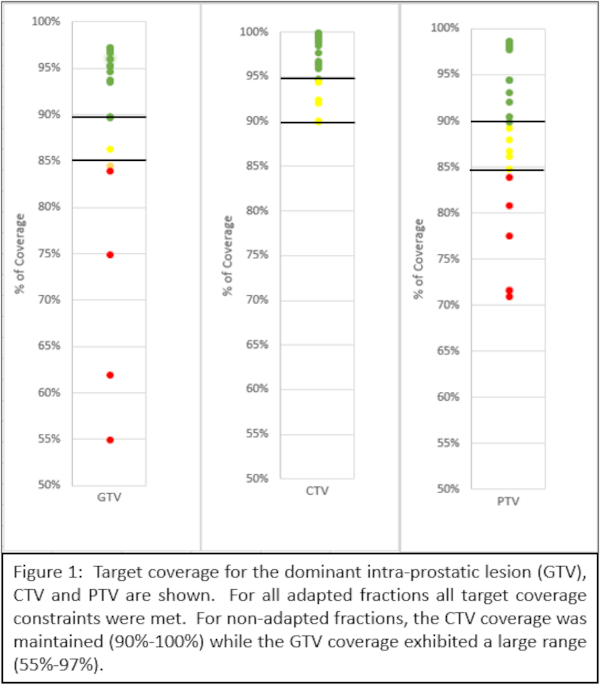
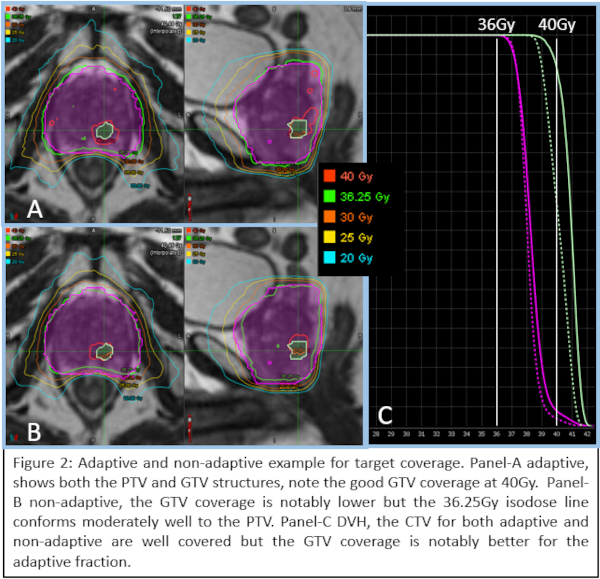
For non-adapted fractions the GTV coverage ranged
from 55-97% at the boost dose level, where 14/20 fractions had 90% or more
coverage. All
adapted fractions had greater than 90% coverage. For non-adapted fractions the CTV coverage ranged from 90-100%, where 18/25
fractions had greater than 95% coverage. The CTV coverage was 98% or greater
for all adapted fractions. For the
non-adapted fractions the PTV coverage ranged from 71-99%, while for the PTV
coverage constraint was met for all adapted fractions. Very few OAR constraints
were exceeded in the non-adaptive setting, and none were exceeded in the
adaptive setting. The anorectum constraint was exceeded 1/25 fractions and the
bladder constraint was exceeded 3/25 fractions.
Conclusion
Online adaptive MR-Guided
SBRT of prostate cancer using daily re-optimization resulted in better target coverage
as compared with non-adaptive SBRT, this was especially true for the GTV where
the non-adaptive coverage ranged from 55%-97%. Generally, the OARs fared well
in the non-adaptive setting with moderately increased sparing for adaptive
fractions.