Early and late treatment toxicity of post-prostatectomy irradiation
PO-1398
Abstract
Early and late treatment toxicity of post-prostatectomy irradiation
Authors: Marcin Miszczyk1, Monika Szołtysik1, Maja Hasterok1, Bartłomiej Goc2, Donata Gräupner2, Paweł Rajwa3,4, Konrad Rasławski2, Iwona Jabłońska1, Łukasz Magrowski1, Oliwia Masri1, Wojciech Majewski1
1Maria Sklodowska-Curie National Research Institute of Oncology, IIIrd Radiotherapy and Chemotherapy Department, Gliwice, Poland; 2Maria Sklodowska-Curie National Research Institute of Oncology, Radiotherapy Department, Gliwice, Poland; 3Comprehensive Cancer Center, Vienna General Hospital, Medical University of Vienna, Department of Urology, Vienna, Austria; 4Medical University of Silesia, Department of Urology, Zabrze, Poland
Show Affiliations
Hide Affiliations
Purpose or Objective
While prostate
cancer treatment is increasingly effective its toxicities remain a great
concern. In this study, we report on the adverse events (AE) of
post-prostatectomy irradiation based on our institutional experience, review
the reproducibility of organs-at-risk (OAR) contouring, and finally investigate
the association of various dose-volume parameters with treatment sequelae.
Material and Methods
We included 167 consecutive patients who had received post-prostatectomy
radiotherapy (either adjuvant or salvage) to the prostatic bed with or without
pelvic node irradiation. The medical history was reviewed for AE, which were
scored according to the CTCAE v.5.0 AE reporting guidelines. The rectum and
bladder organs-at-risk were contoured anew, based on the treatment planning
computed tomography, following RTOG/NRG Guidelines. The volumes were then
compared with the original contours and analyzed based on dose-volume histogram
(DVH) values using ROC curves. Kaplan-Meier curves were used to estimate the cumulative
rate of toxicity at given time-points (3 months and 5 years).
Results
The median patients’ age was 63.2 (IQR 58.8 – 67.5), and the median
follow-up was 51 months (IQR 22.4-97.1). Grade 2 or higher urinary tract
toxicity occurred in 13.3% and 28.2% of the patients at 3 months and 5-years,
respectively. A total of 17 (10.2%) patients experienced grade 3 or higher
toxicity within the follow-up, most commonly (8.4%) associated with urinary
tract obstruction requiring surgical intervention. Grade 2 or higher rectal
toxicity occurred in 7.2% and 13.9% of the patients at 3 months and at 5 years.
Grade 3 or higher rectal toxicity was much less frequent; reported in 2.4% of
patients.
There was a trend towards a
lower volume of the new rectal contours, as compared to the originally
delineated organ, which was found in a majority of the patients (74.9%). The
new contours were smaller by a median of 16.5% (IQR 8-28.5). The bladder
contours were comparable in approximately 50.9% of patients, and in the majority
(83.5%) of the remaining patients, the difference compared to the initial OAR
volume was low (<10%).
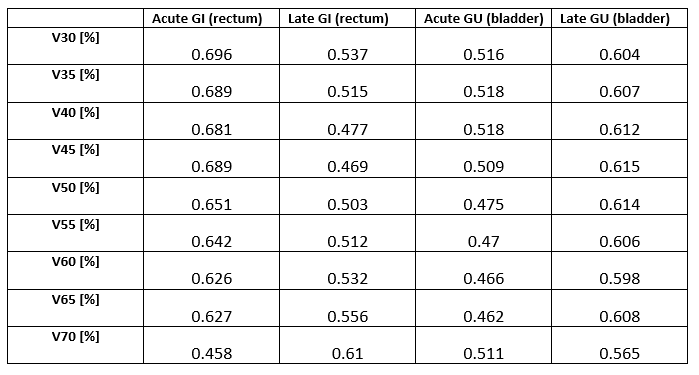
Table 1 presents the association between consecutive
dose-volume parameters and grade II or higher rectal and urinary AEs. The
presented values, however, did not reach statistical significance.
Table 1. AUC values in ROC analysis
of selected DVH parameters for the occurrence of grade II or higher GI or GU
toxicity. Vx represents the volume (%) of OAR receiving a dose of at least x Gy.
Conclusion
Our analysis suggests that the
rectal contours might often be overestimated, which can result in a bias
towards accepting higher doses to the rectum when assessing dose-volume
parameters. Moreover, the overall treatment toxicity of post-prostatectomy
radiotherapy seems to be not neglectable, especially in terms of significant urinary
tract adverse events such as urinary tract obstruction.