Organ preservation with tri-modality in bladder Ca- Experience from a Cancer institute in LMIC
Muneeb Uddin Karim,
Pakistan
PO-1386
Abstract
Organ preservation with tri-modality in bladder Ca- Experience from a Cancer institute in LMIC
Authors: Muneeb Uddin Karim1, Aqueel Shahid2, Maryam Inayat2, Muhammad Atif Mansha2, Taskheer Abbas2, Sumera Butt2
1Shaukat Khanum Memorial Cancer Hospital & Research Centre , Clinical & Radiation Oncology, Lahore, Pakistan; 2Shaukat Khanum Memorial Cancer Hospital & Research Centre, Clinical & Radiation Oncology, Lahore, Pakistan
Show Affiliations
Hide Affiliations
Purpose or Objective
Neoadjuvant cisplatin-based chemotherapy followed by radical cystectomy is the gold standard for the treatment of muscle-invasive bladder Ca. However, the gold standard may not be the best treatment for individual patients. The alternative best treatment option is the bladder sparing tri-modality treatment in which surgery (maximal TURBT) is followed by definitive chemoradiation therapy with the intent of cure along with organ preservation.
Our primary objective includes the estimation of the overall survival and disease-free survival at 3 and 5 years in patients of bladder cancer treated
with a bladder preservation approach at a dedicated cancer institute.
Secondary objectives include the outcome of different radiation fractionation, induction chemotherapy and time to radiation after TURBT.
Material and Methods
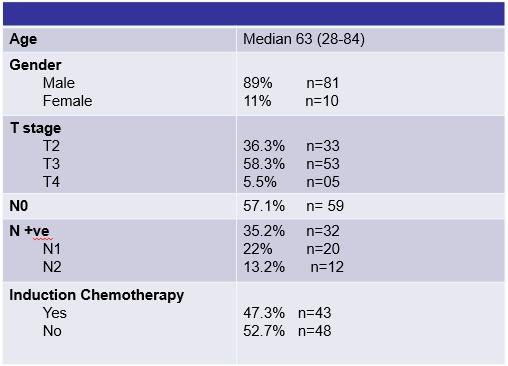
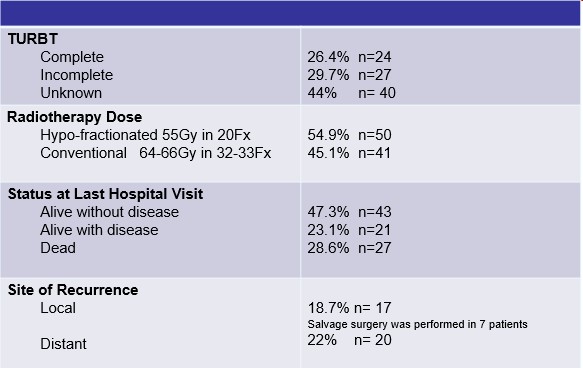
After taking IRB approval, 91 patients of bladder
cancer treated with curative intent and bladder preservation approach, between
January 2010 till December 2018 were
retrospectively reviewed. Demographic characteristics and details of all
procedures including surgery (TURBT), chemotherapy and radiation therapy were
documented with the help of the Hospital Information System. Treatment response and
follow-up details were documented according to notes.
Results
The median age was 63 (range 28-84). 89% (n=80) were
male. Out of 91 patients, 53 (58%) patients had T3 disease and 32 (35%) of the
patients had node-positive disease. Induction chemotherapy was given in 43
patients (47.3 %) after TURBT. 78 (85.7%) patients received concurrent
chemotherapy with radiation therapy. Hypo-fractionated radiation therapy (55Gy
in 20 fractions) was given in 50 patients (54.9%). Overall survival was found
to be 77% and 62% and DFS was 62% and 51% at 3 and 5 years respectively. Induction chemotherapy had no
significant impact on OS. However, OS was estimated to be higher in those
patients in which radiation therapy was started within 6 weeks of TURBT and in
those patients who received hypofractionated radiotherapy.
Conclusion
Our study shows that bladder preservation therapy is an
effective approach that can be the best treatment in selected patients with
Bladder Ca. Overall survival at 3 and 5
years in patients treated with bladder preservation approach at our institute
is comparable to the standard of care (radical cystectomy). We recommend case
discussion in a Multidisciplinary site-specific tumour board which is important and
necessary for offering organ preservation to the bladder ca patients.