HYPOFRACTIONATED RADIOCHEMOTHERAPY IN CERVICAL CANCER: A PRELIMINAR EXPERIENCE
PO-1333
Abstract
HYPOFRACTIONATED RADIOCHEMOTHERAPY IN CERVICAL CANCER: A PRELIMINAR EXPERIENCE
Authors: BIANCA SANTO1, Donatella Russo1, Maria Cristina Barba1, Elisa Cavalera1, Elisa Ciurlia2, Paola De Franco1, Giuseppe Di Paola1, Angela Leone3, Antonella Papaleo1, Daniela Musio1
1Vito Fazzi Hospital, Radiation Oncology, LECCE, Italy; 2VCito Fazzi Hospital, Radiation Oncology, LECCE, Italy; 3Viton Fazzi Hospital , Radiation Oncology, LECCE, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate
feasibility and tolerability of hypofractionated external beam radiation
therapy (EBRT) schedule with concurrent chemotherapy (weekly cisplatin 40mg/m2)
in high volume and node positive cervical cancer (CC).
Material and Methods
From March 2018 to
July 2020, 15 consecutive patients, median age 59 (47-80) with locally advanced
(IIB-IVa) high volume CC received exclusive chemoradiation. Hypofractionated
EBRT was delivered using VMAT and a simoultaneous integrated boost. EBRT
schedule was 66.08 Gy to primary, 59.92 Gy to positive nodes, 54.4 Gy to
negative pelvic nodes and 50.4 Gy to lomboaortic nodes, when required, in 28
daily fractions. Pelvic RM was performed during the last week of EBRT to
evaluate tumor response. Four patients received image guided brachytherapy
boost (BRTb) (14 Gy in 2 weekly fractions), in 3 patients BRTb was technically
not feasible, 2 patients were unfit to continue treatment, in 4 elderly
patients BRTb was not planned. In 2 non responders patients, systemic therapy
followed chemoradiation. Cone beam CT was acquired daily.
Acute and late toxicity were registered using
RTOG scales.
Results
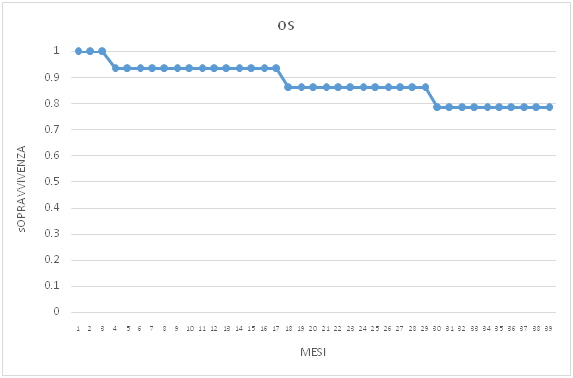
Median follow-up is
18.7 months (0.33-38). The oldest patient of the series (80 years) died early
for a cardiovascular event. Other 3 patients died after 17, 45 and 50 months
respectively. Eleven patients are alive, 10 without evident disease and one is
lost at follow-up. Overall survival is shown in fig.1.
Acute genitourinary (GU) and gastroenteric (GI)
toxicity was ≤ G2 and all patients completed treatment in 8 weeks.
Late GU toxicity ≥ G3 was reported in patients
who received BRT boost (in 2 patients G3 and in 1 patient G4, requiring
temporary colostomy). No patients presented > G2 late GI toxicity.
Fig.1 Overall survival
Conclusion
At state of art,
brachytherapy is mandatory within cervical cancer radiation strategies. A dose
escalation with EBRT could provide to a tumor downsizing useful when only
endocavitary without combined interstitial brachytherapy is available but
insufficient to cover high volume residual primary.
Unfortunately, in our series, hypofractionated
EBRT plus BRT it's more toxic than standard treatment.
Moreover, in elderly patients or in patients
with technical impossibility to receive BRT, external dose escalation could
represent an alternative and this schedule seems to be useful in local control.
More trials including higher number of patients are necessary to define the real role of hypofractionation in cervical cancer.