Radical chemoradiotherapy for cervical cancer: current practice and avenues for future investment
Orla Houlihan,
United Kingdom
PO-1330
Abstract
Radical chemoradiotherapy for cervical cancer: current practice and avenues for future investment
Authors: Orla Houlihan1,2, Monica Byrne3, Geraldine Workman3, Sergio Esteve3, Ursula McGivern1, Anne Drake1, Elizabeth Baird1
1Northern Ireland Cancer Centre, Belfast City Hospital, Clinical Oncology, Belfast, United Kingdom; 2Queen's University Belfast, School of Medicine, Dentistry and Biomedical Sciences, Belfast, United Kingdom; 3Northern Ireland Cancer Centre, Belfast City Hospital, Radiotherapy Medical Physics, Belfast, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Recent
technological advances have taken place in the non-surgical treatment of
cervical cancer. We conducted a review of current practice in our institution
with the view to informing future investment in resources.
Material and Methods
A
retrospective review of consecutive women treated with external beam
radiotherapy (EBRT) and high dose rate brachytherapy for cervical cancer
between November 2017 and November 2019 was performed. Data regarding patient
demographics, tumour characteristics, chemotherapy, radiotherapy and outcomes
were collected from patient charts and radiotherapy records and analysed using
GraphPad Prism 9.2.0.
Results
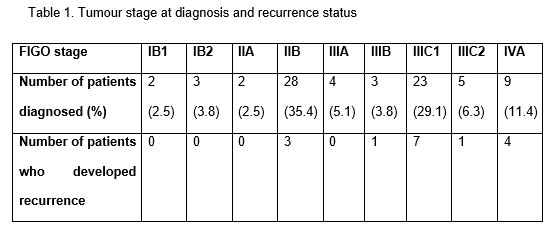
Seventy
nine women met inclusion criteria for the study. Mean age was 47 years (range
24-78 years). More than half of patients had FIGO stage IIB (n=28; 35.4%) or
FIGO stage IIIC1 (n=23; 29.1%) disease (Table 1). Nine patients experienced
grade 3 or higher bowel toxicity, of whom the mean cumulative (EBRT plus
brachytherapy) minimum biologically equivalent dose in 2 Gy fractions to the
most irradiated 2cc (EQD2 D2cc) of bowel was ≥ 65 Gy for seven patients. Sixteen
patients (20.3%) developed local and/or distant disease recurrence, three of
whom had parametrial involvement (FIGO stage IIB), and the remainder who had
locally advanced disease of at least stage IIIB (Table 1). Mean HRCTV D90 (the
minimum dose covering 90% of the high risk clinical target volume) for those
patients who developed a recurrence was lower at 84.6 Gy (standard deviation
(SD) 12.1 Gy) than the mean HRCTV D90 of 96.5 Gy (SD 14.5 Gy) for those
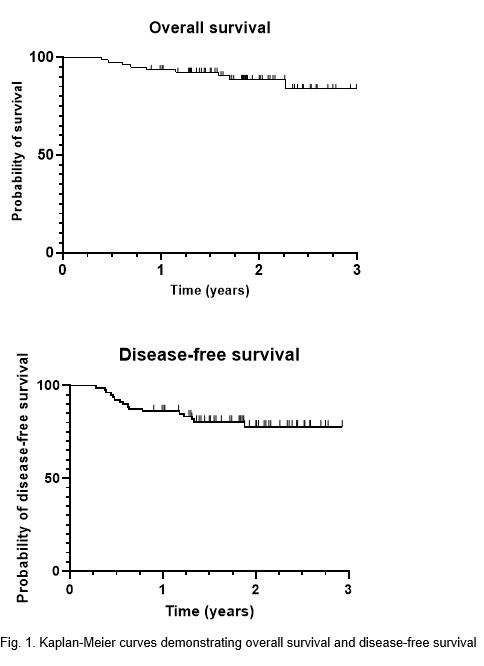
patients who did not develop a recurrence. At two years, overall survival was
88% and disease-free survival was 78% (Fig. 1).
Conclusion
Outcomes
in our institution were comparable with published studies. The addition of
interstitial brachytherapy to our practice may improve outcomes for patients
with locally advanced, bulky disease. In vivo dosimetry would be useful
to monitor radiation dose and radioactive source location in real-time during
brachytherapy given the potential for movement of the target and organs at risk.