Narrowing the difference in dose delivery for IOERT and IOBT for rectal cancer
An-Sofie Verrijssen,
The Netherlands
PO-1323
Abstract
Narrowing the difference in dose delivery for IOERT and IOBT for rectal cancer
Authors: An-Sofie Verrijssen1, Cathryn Huibregtse Bimmel-Nagel1, Jeltsje Cnossen1, Jacqueline Theuws1, Heike Peulen1, Hetty van den Berg1, Dorien Rijkaart1, Elke Voogt2, Pim Burger2, Harm Rutten2,3, Wim Dries1
1Catharina Hospital, Radiotherapy, Eindhoven, The Netherlands; 2Catharina Hospital, Surgery, Eindhoven, The Netherlands; 3GROW School for Oncology and Developmental Biology, Maastricht University, Surgery, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
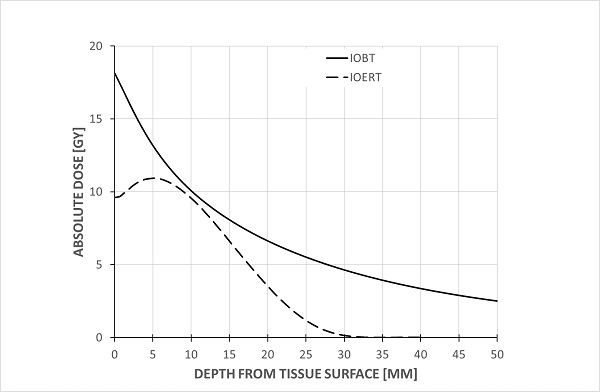
Purpose or Objective
Intraoperative radiotherapy (IORT) has been used as a tool to provide a high dose radiation boost to a limited volume in patients with locally advanced or recurrent rectal carcinoma who have fixed tumors with a likelihood of microscopically involved resection margins, in order to improve local control. The two main techniques to deliver IORT are through High Dose Rate (HDR) Brachytherapy, termed Intraoperative Brachytherapy (IOBT), and through electrons, termed Intraoperative Electron Radiotherapy (IOERT), both having very different dose distributions. A recent paper described an improved local recurrence-free survival favoring IOBT over IOERT for patients with locally advanced or recurrent rectal cancer and microscopically irradical resections. Although several factors may have contributed to this result, an important difference between the two techniques is the higher surface dose delivered by IOBT. This article describes an adaptation of the IOERT technique at the Catharina Cancer Institute (CCI) (Eindhoven, NL) to achieve a comparable surface dose as the dose delivered by IOBT.
Material and Methods
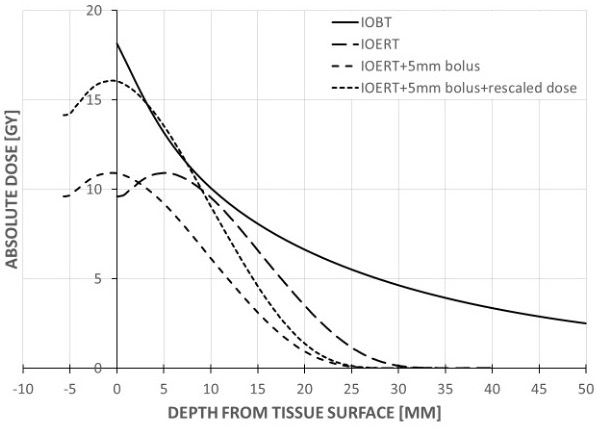
Two steps are taken to increase the surface dose for IOERT: 1) Introducing a bolus to achieve a maximum surface dose, and 2) re-normalizing in order to allow for the same prescribed dose at the reference depth.
Results
By realizing these adaptations, the dose delivery curve approaches that of IOBT in the most superficial millimeters of irradiated tissue. In greater depths, the dose fall-off is steeper than that of IOBT. The effect of this adaptation on local control will be analyzed in five years by comparing patients treated with a historical cohort. We expect no increased toxicity due to this adaptation. Patients treated at the IOBT center have acceptable toxicity despite this high surface dose, and as stated electron dose fall-off remains steeper in comparison to IOBT dose-fall off, possibly resulting in less toxicity with IOERT.
Due to the fixed tube used for IOERT, one of the disadvantages of IOERT when compared to IOBT is the relative inability to adapt to the anatomy of the patient. Two possible bevel angles (30 and 45 degrees) can be used, depending on the shape of the target volume. With the use of the bolus and re-normalization, we are able to compensate for differences in anatomy while still being able to deliver a high surface dose with a steep dose fall-off.
Conclusion
We describe and propose an adaptation of the IOERT technique in order to increase surface dose with the aim of further improving local control. The dosimetric differences between IOERT and IOBT are reduced thanks to this adaptation.