Impacts and consequences of spleen irradiation after adjuvant chemoradiation for stomach cancer
Shing Fung Lee,
Singapore
PO-1306
Abstract
Impacts and consequences of spleen irradiation after adjuvant chemoradiation for stomach cancer
Authors: Shing Fung Lee1,2, Pui Lam Yip3, Aray Wong3, Francesca Ng2, Vicky Koh4, Lea Choung Wong4, Francis Ann Shing Lee2, Harvey Mamon5
1University of Hong Kong, Department of Clinical Oncology, Hong Kong, Hong Kong (SAR) China; 2Tuen Mun Hospital, Department of Clinical Oncology, Hong Kong, Hong Kong (SAR) China; 3Tuen Mun Hospital, Department of Clinical Oncology, Hong Kong, Hong Kong (SAR) China; 4National University Cancer Institute, Department of Radiation Oncology, Singapore, Singapore; 5Dana-Farber/Brigham and Women's Cancer Center, Harvard Medical School, Department of Radiation Oncology, Boston, Massachusetts, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
To determine whether severity of lymphopenia is associated
with the dose-volume histogram (DVH) parameters of the spleen irradiated unintentionally
during adjuvant chemoradiation (CRT) in patients with gastric cancer.
Material and Methods
Patients who received adjuvant chemoradiation for
gastric cancer from January 2015 to December 2020 were analyzed. The splenic DVH
parameters were reported as mean splenic dose (MSD) and percentage of splenic
volume receiving at least x Gray (Gy). Peripheral blood counts were recorded at
baseline and after CRT. The development of severe post-CRT lymphopenia (absolute
lymphocyte count [ALC] <0.5 K/μL) was assessed by multivariable logistic
regression with use of patient and dosimetric factors. Overall survival (OS), recurrence-free
survival (RFS), and cumulative incidence of infectious events were estimated and
analyzed with the use of stepwise Cox model or competing risk analysis as
appropriate.
Results
We analyzed 84 patients, with median follow-up
duration of 42 months. The median baseline ALC and
post-CRT ALC were 1.9 K/μL (range, 0.7–2.8 K/μL) and 0.9 K/μL (range, 0.0–4.9 K/μL),
respectively (P < 0.001). MSD
> 40 Gy (odd ratio [OR], 3.81; 95% confidence interval [CI], 1.15–12.60;
P = 0.028), high baseline
neutrophil-to-lymphocyte ratio (OR per 1 unit increase, 2.13; 95% CI, 1.02–4.41;
P = 0.043), and sex (OR for male to female, 0.34; 95% CI, 0.12–0.97; P
= 0.043) were associated with the
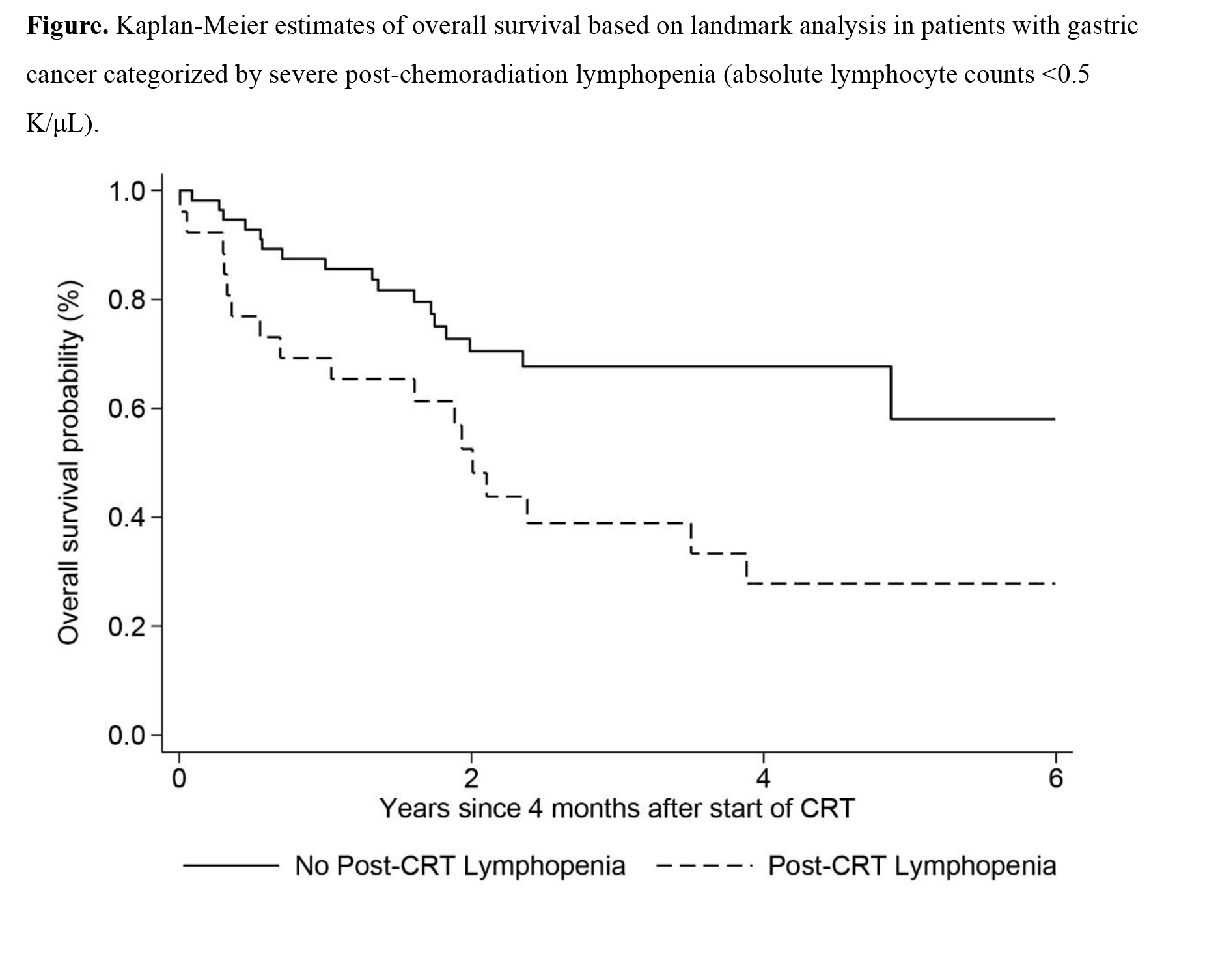
development of severe post-CRT lymphopenia, which was a risk factor for poorer
OS (hazard ratio [HR], 2.27; 95% CI, 1.13–4.58; P = 0.022) and RFS (HR, 2.21; 95% CI, 1.13–4.32;
P = 0.021). The cumulative incidence of infections was higher among
patients with severe post-CRT lymphopenia (2.53, 95% CI, 1.03–6.23, P
= 0.043).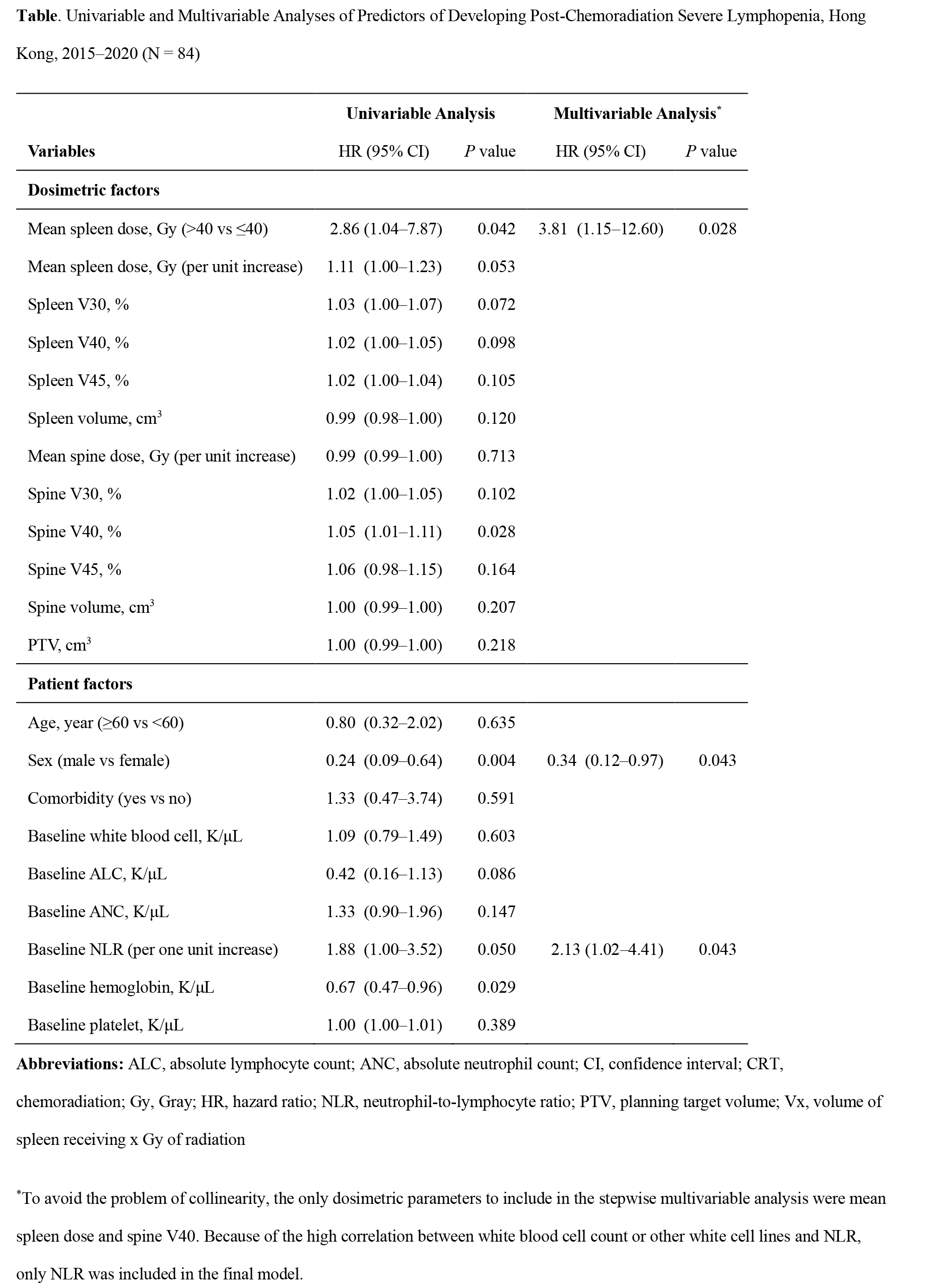
Conclusion
Higher splenic radiation doses increase the odds of
severe post-CRT lymphopenia, which is common and is an independent predictor of
poorer OS and higher risks of recurrence and infections in gastric cancer
patients receiving adjuvant CRT. Considering the spleen as an organ-at-risk and
optimizing the splenic DVH parameters before plan evaluation may decrease the
risk of severe post-CRT lymphopenia.