Muscle Loss After Stereotactic Body Radiotherapy Predicts Worse Survival in Hepatocellular Carcinoma
Jen-Fu Yang,
Taiwan, Province of China
PO-1305
Abstract
Muscle Loss After Stereotactic Body Radiotherapy Predicts Worse Survival in Hepatocellular Carcinoma
Authors: Jen-Fu Yang1, Cheng-Hsiang Lo1, Meei-Shyuan Lee2, Chun-Shu Lin1, Po-Chien Shen1, Yang-Hong Dai1, Ying-Fu Wang1, Wen-Yen Huang1
1Tri-Service General Hospital, Department of Radiation Oncology, Taipei, Taiwan; 2National Defense Medical Center, School of Public Health, Taipei, Taiwan
Show Affiliations
Hide Affiliations
Purpose or Objective
The relationship between sarcopenia and treatment outcomes, especially in patients with hepatocellular carcinoma (HCC) undergoing stereotactic body radiotherapy (SBRT) has not been well-explored. This study aimed to investigate the effects of sarcopenia on the survival and toxicity after SBRT in patients with HCC.
Material and Methods
We included 137 patients with HCC treated with SBRT at our institution between 2008 and 2018. Sarcopenia was defined as a skeletal muscle index (SMI) of < 49 cm2/m2 for men and < 31 cm2/m2 for women using pre- and post-SBRT computed tomography images at the mid-level of the third lumbar vertebra. The SMI change was presented as the standardized value (change per 90 days). The Kaplan–Meier method was used for survival estimation, and the Cox proportional hazards regression model was used to determine prognosticators for survival.
Results
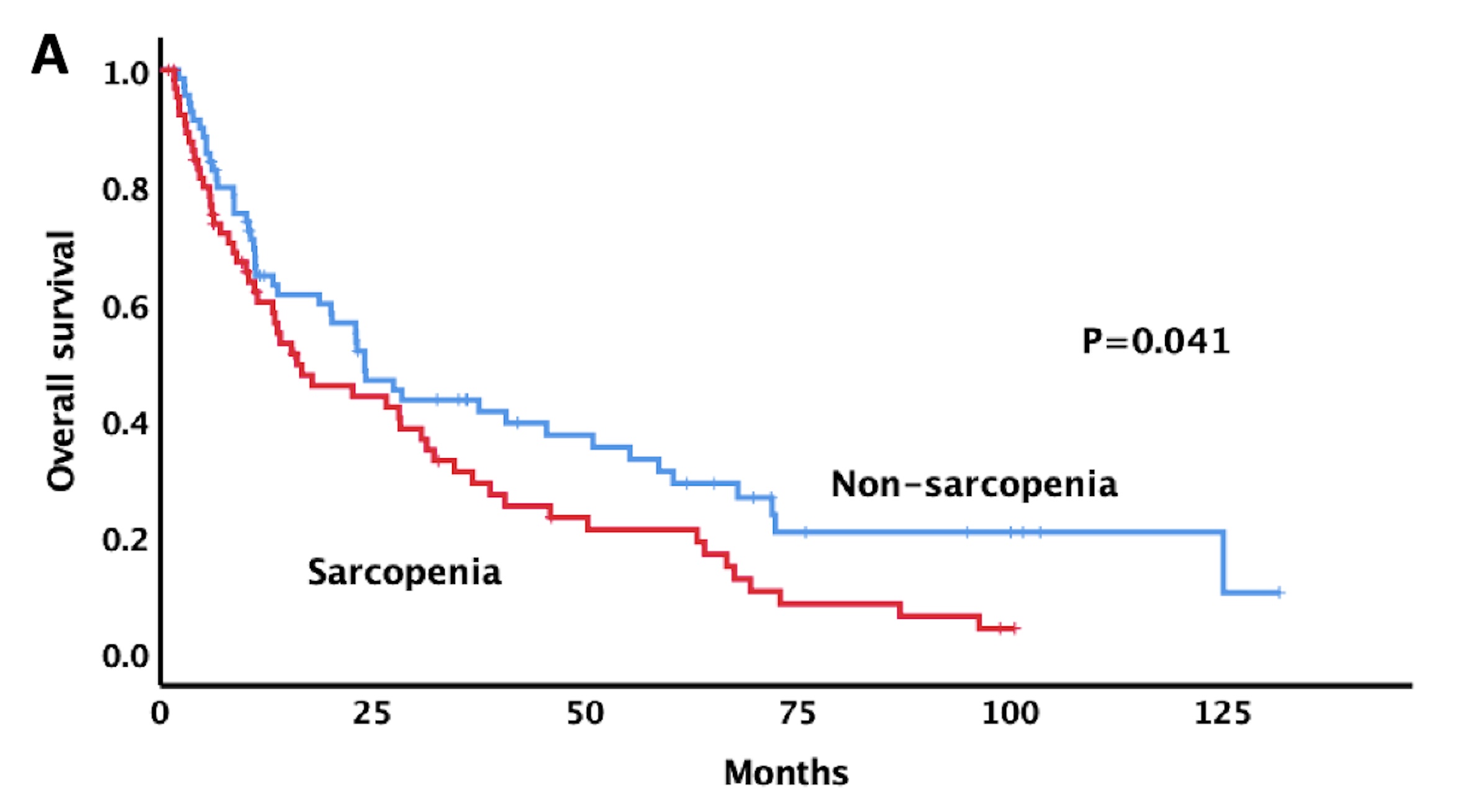
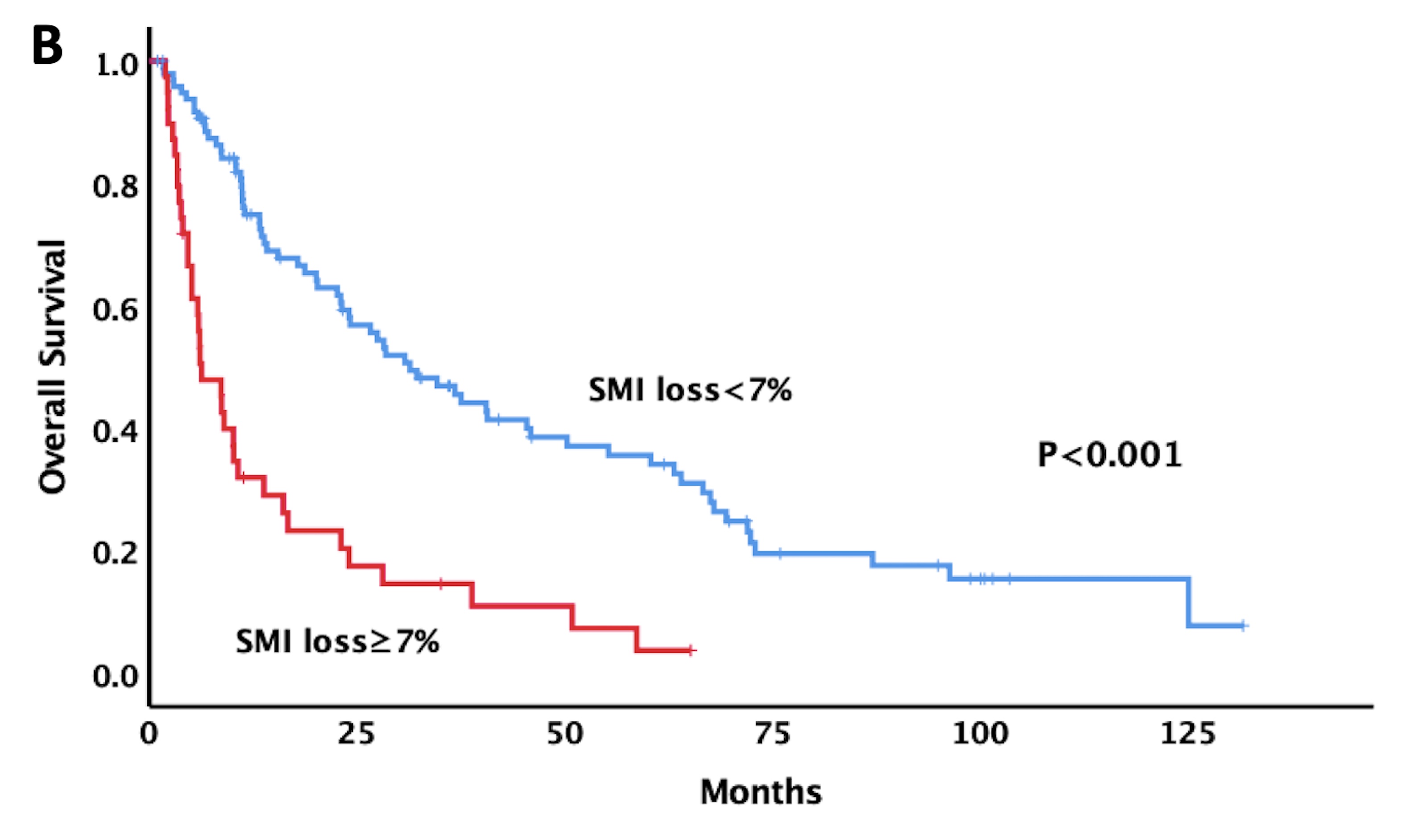
Sarcopenia was present in 67 of 137 eligible patients. With the median follow-up of 14.1 months and 32.7 months in the entire cohort and in those alive, respectively, patients with pre-SBRT sarcopenia or SMI loss ≥ 7% after SBRT had worse overall survival than their counterparts (figure). Significant predictors associated with survival on Cox multivariate analysis were SMI loss ≥ 7% after SBRT, presence of extrahepatic metastasis, neutrophil-to-lymphocyte ratio, and multiple tumors. Separate Cox models according to the absence and presence of pre-SBRT sarcopenia showed that SMI loss ≥7% remained a significant survival predictor in patients with sarcopenia compared with those without sarcopenia. SMI loss ≥ 7% is also a predictor of the Child-Pugh score increase by ≥ 2 points after SBRT.
Conclusion
SMI loss ≥ 7% after SBRT is a significant prognostic factor for worse survival and is associated with liver toxicity compared with pre-SBRTsarcopenia.