Hemostatic Radiotherapy for Gastric Cancer: Relationship Between MR Images and Tumor Markers
PO-1296
Abstract
Hemostatic Radiotherapy for Gastric Cancer: Relationship Between MR Images and Tumor Markers
Authors: Osamu Tanaka1, Nobuaki Yagi2, Masahiro Tawada3, Takuya Taniguchi1, Kousei Adachi1, Shuto Nakaya1, Chiyoko Makita4, Masayuki Matsuo5
1Asahi University Hospital, Department of Radiation Oncology, Hashimoto-Cho, Gifu city, Japan; 2Asahi University Hospital, Department of Gastroenterology, Hashimoto-Cho, Gifu city, Japan; 3Asahi University Hospital, Department of Surgery, Hashimoto-Cho, Gifu city, Japan; 4Gifu University Hospital, Department of Radiation Oncology, 1-1 Yanagido, Gifu, Japan; 5Gifu University Hospital, Department of Radiation Oncology, 1-1 Yanagido, Gifu city, Japan
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy
(RT) has a hemostatic effect on gastric cancer. A response rate of 80% was obtained when
patients were treated with RT at a dose of 20 Gy in 5 daily fractions (20 Gy/5
fx). Endoscopy is the first choice for the pretreatment diagnosis and the
post-treatment evaluation of gastric cancer. However, in recent years, an
increasing number of studies have reported that diffusion-weighted magnetic
resonance imaging (DW-MRI) is useful for preoperative staging. The apparent diffusion
coefficient (ADC; unit: 10−3 mm2/sec) is a quantitative
value. But until now, endoscopic
findings and tumor markers, such as carcinoembryonic antigen (CEA; unit:
ng/ml), obtained via blood tests, have been used to judge the therapeutic
effects of treatment. No studies have investigated
the relationship between the ADC value as a diagnostic image and the CEA value
as a blood diagnostic measure before and after RT. This study aimed to clarify
the relationship between ADC and tumor markers (e.g., CEA) to obtain more
accurate gastric cancer information noninvasively by combining data from blood
and imaging tests.
Material and Methods
Out of
21 patients who received hemostatic RT for gastric cancer from 2019 to 2021, 8
eligible patients completed the protocol. Patients with bleeding as identified by pathological and endoscopic
examinations and those with hemoglobin levels of ≤8 g ml−1 at the
initial consultation were included. We
obtained the following values: the measured CEA value, the measured ADC value, the
ratio of the ADC values before and 1 (or 3) month(s) after RT, and the ratio of
the CEA values before and 1 (or 3) month(s) after RT. We evaluated the changes
in the ADC and CEA values in a chronological order—before and 1 (or 3) month(s)
after RT. We also compared the ratio of the ADC values and the ratio of the CEA
values before RT, 1 month after RT, and 3 months after RT.
Results
The CEA values showed a
statistically significant decrease from before RT to 1 month after RT, but no
statistically significant change was observed between 1 month and 3 months
after RT. The ADC values showed a
statistically significant increase from before RT to 1 month after RT but
decreased 3 months after RT compared with 1 month after RT.
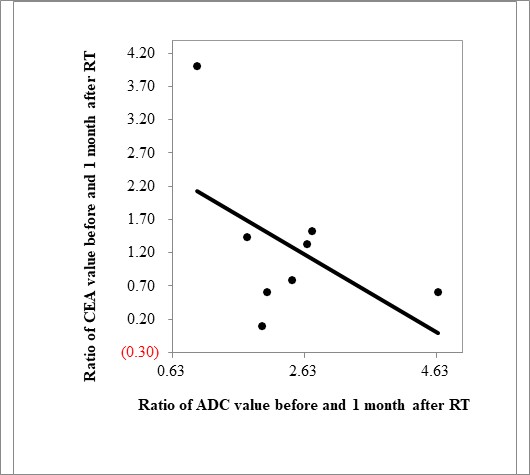
The
ratio of ADC (1
month after RT/before RT) and the
ratio of CEA
showed an inverse correlation
(r =
−0.519).
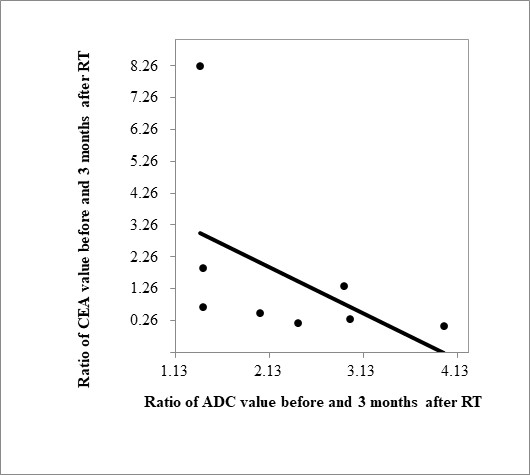
Similarly, the ratio of ADC (3 months after RT/before RT) and the ratio of CEA showed an inverse correlation
(r =
−0.499).
Conclusion
The usefulness of DW-MRI has
been reported mainly for solid tumors. Herein, we evaluated the usefulness of
DW-MRI for gastric cancer using a tumor marker in RT settings. We
showed that changes in the ADC and CEA values are correlated
using ratios (before/1 and 3 months after RT).
Additionally, 3 months after RT, a decrease in the ADC value appeared earlier
than a decrease in the CEA value. Our findings thus suggest that ADC may
represent biological changes earlier than CEA.