Stereotactic radiotherapy after chemotherapy in patients with locally advanced pancreatic cancer
PO-1292
Abstract
Stereotactic radiotherapy after chemotherapy in patients with locally advanced pancreatic cancer
Authors: Charlotte LE ROY1, Rémy Barbe1, Roger Sun1, Pascal Burtin1, Maximiliano Gelli1, Eric Deutsch1, Jérôme Durand-Labrunie1
1Institut Gustave Roussy, Radiation Oncology, VILLEJUIF, France
Show Affiliations
Hide Affiliations
Purpose or Objective
We
aimed to report the efficacy and tolerance of Stereotactic Body Radiation
Therapy (SBRT) after induction chemotherapy (ICT) for the treatment of
unresecable locally advanced pancreatic cancer (LAPC).
Material and Methods
We
performed a single-institution retrospective review of patients with LAPC treated
with SBRT after ICT from 2015-2020. The median dose was 37.5 Gy (range: 32.5 -
40 Gy) in five fractions. Most patients were treated by mFOLFIRINOX followed by
CyberKnife robotic SBRT using fiducial markers for tracking. Median
prescription isodose was 77% (range: 74 – 78). Coverage of the target volume at
the prescribed dose was degraded in order to comply with dose constraints to
organs at risk. Endpoints included local control, progression free survival,
overall survival, and toxicity calculated from the date of radiological
diagnosis. All baseline and follow up CT scans were reviewed by an independent
radiologist using RECIST 1.1 criteria. Each progression has been classified
according to location: in-field, marginal, or out-field.
Results
Fifty-two
patients were treated, with a median follow-up of nineteen months. All
pancreatic tumors were adenocarcinoma assessed to be non resectable LAPC. The 1
and 2 year-local-control rates after ICT and SBRT were 71% and 21% respectively
with a median local control of 22.7 months (Figure 1). Progression free
survival at 1 and 2 years were 61% and 13%, and overall survival rates were 83%
and 35% at 1 and 2 years respectively. About half of patients experienced acute
toxicity and 13.4% a late toxicity. Grade 3-4 acute toxicities were experienced
by 3.8% of patients, the most common being abdominal pancreatic pain. Grade 3-4
late toxicities were experienced by 7.7% of patients, the most common being
gastrointestinal perforation, with one treatment related death. Majority of patients
declared a distant or outfield relapse (46.2%), compared to marginal or
in-field recurrence (17.3% and 28.8% respectively) (figure 2).
Figure 1.
Overall Survival - Local control - Progression free-survival,from diagnosis
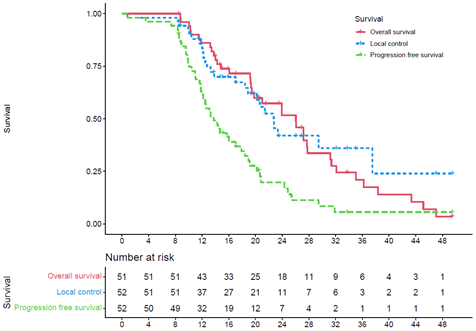
Figure 2.
Recurrences’ profil types

Conclusion
Chemoradiotherapy
has shown a benefit in terms of local control in LAPC after ICT, without
benefit in survival. Our results suggest that SBRT may be considered as an
alternative option with a much shorter treatment time and less acute toxicity
for equivalent local control and acceptable late toxicity.