Skeletal muscle measured at T12 is a prognostic biomarker in oesophageal cancer patients
Donal McSweeney,
United Kingdom
PO-1286
Abstract
Skeletal muscle measured at T12 is a prognostic biomarker in oesophageal cancer patients
Authors: Donal McSweeney1, Ganesh Radhakrishna2, Andrew Green1, Paul A. Bromiley3, Marcel van Herk1, Alan McWilliam1
1University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom; 2The Christie NHS Foundation Trust, Department of Medical Oncology, Manchester, United Kingdom; 3University of Manchester, Division of Informatics, Imaging and Data Sciences, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Sarcopenia is emerging as a prognostic factor for multiple patient
groups treated with radiotherapy (RT) where it is associated with increased
toxicity and decreased overall survival. Sarcopenia is typically assessed via
the skeletal muscle index (SMI): skeletal muscle area at L3 normalised by
patient height. Therefore, cohorts where routine imaging does not include L3
are often neglected.
Patients with oesophageal cancer are known to experience malnutrition
and weight loss, associated with poorer outcomes. In this work, we explore the utility
of SMI, measured at T12, as a prognostic factor in patients with oesophageal
cancer treated with concurrent chemoradiotherapy (CCRT). We then compare sarcopenia
with other measures of patient frailty: performance status (PS) and body mass
index (BMI).
Material and Methods
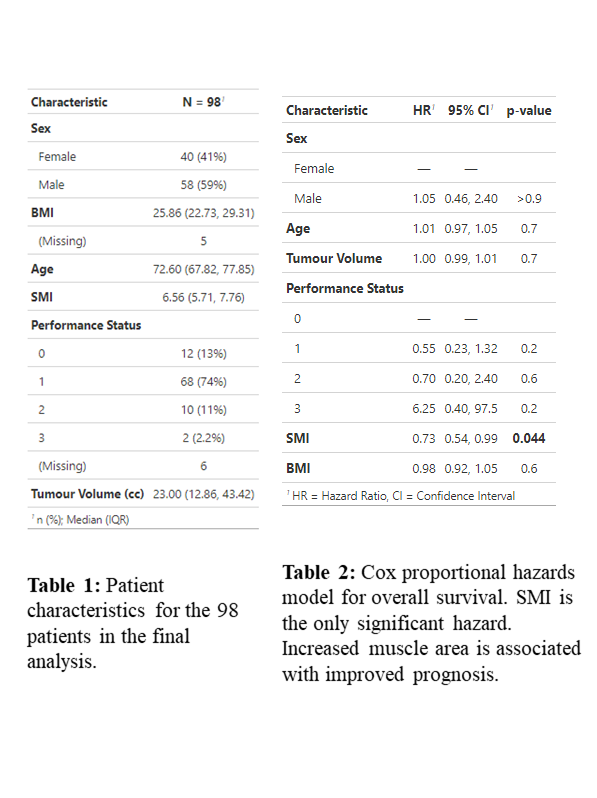
103 patients with oesophageal cancer treated with CCRT, 50Gy in 25
fractions, were retrospectively collected. Patient characteristics are shown in
Table 1. T12 was manually identified
on RT planning scans. An in-house artificial intelligence algorithm was then used
to segment the skeletal muscle compartment at T12 and segmentations were
visually assessed for accuracy.
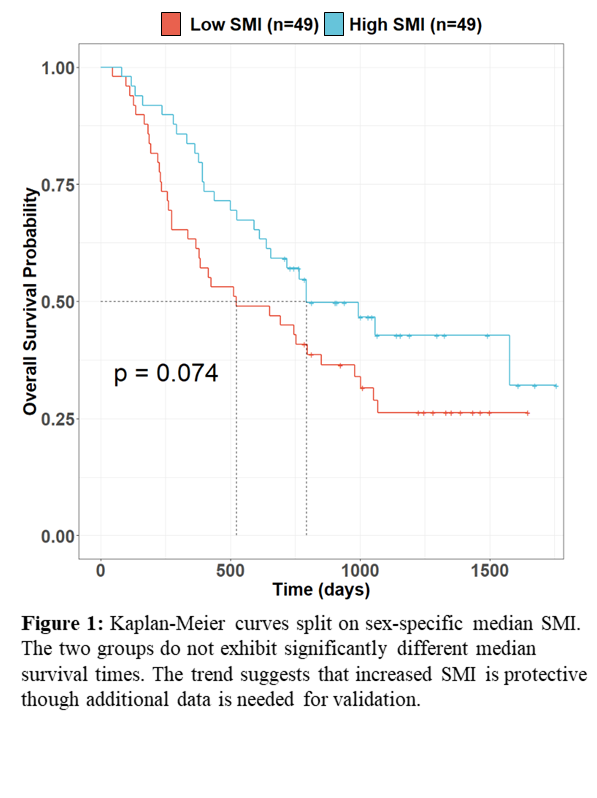
Muscle area was extracted and SMI at T12 calculated for all patients with
successful delineations. Prognostic value was investigated using Kaplan-Meier
curves (split on sex-specific median SMI) and a multivariable Cox model
controlling for biological sex, age, tumour volume, PS and BMI. The
primary endpoint was overall survival.
Results
After removing segmentation failures, 98 patients were available. Kaplan-Meier
curves did not show significant differences in overall survival when split on
sex-specific median SMI (Figure 1; log-rank p=0.074). However,
in multivariable analysis, SMI was significantly associated with survival (HR=0.73,
p=0.044), where a higher SMI seems to be protective (Table 2). The
results suggest that there is an interaction between SMI and other factors in
the multivariable model, showing thatSMI provides additional prognostic information
beyond PS and BMI.
Conclusion
We show that SMI, evaluated at T12 using routine planning scans, is a prognostic
factor in patients with oesophageal cancer treated with CCRT, with increased
muscle mass being protective. Results from our multivariable Cox model show
that SMI provides additional information beyond PS and BMI. Although our results
require further validation, SMI shows promise for patient treatment
stratification.