Early response to chemotherapy as predictor of locoregional and distant failure in NSCLC
PO-1262
Abstract
Early response to chemotherapy as predictor of locoregional and distant failure in NSCLC
Authors: Marie Tvilum1, Marianne Marquard Knap1, Christina Maria Lutz2, Lone Hoffmann2, Azza A. Khalil1, Ate Haraldsen3, Markus Alber4, Cai Grau1,5, Hjørdis Hjalting Schmidt1, Maria Kandi1, Lise Saksø Mortensen1, Marianne Ingerslev Holt1, Ane Appelt6, Ditte Sloth Moeller1
1Aarhus University Hospital, Department of Oncology, Aarhus, Denmark; 2Aarhus University Hospital, Department of Medical Physics, Aarhus, Denmark; 3Aarhus University Hospital, Department of Nuclear Medicine and PET, Aarhus, Denmark; 4Heidelberg University Clinic, Department of Radiation Oncology, Heidelberg, Germany; 5Aarhus University Hospital, Danish Center for Particle Therapy, Aarhus, Denmark; 6University of Leeds, Institute of Medical Research at St James’s, Leeds, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Combined chemo-radiotherapy (cRT) is standard
of care for patients with locally advanced non-small cell lung cancer
(LA-NSCLC). This study evaluates the early radiologic and metabolic tumour response
after chemotherapy and its prognostic value in predicting pattern of failure
for LA-NSCLC-patients.
Material and Methods
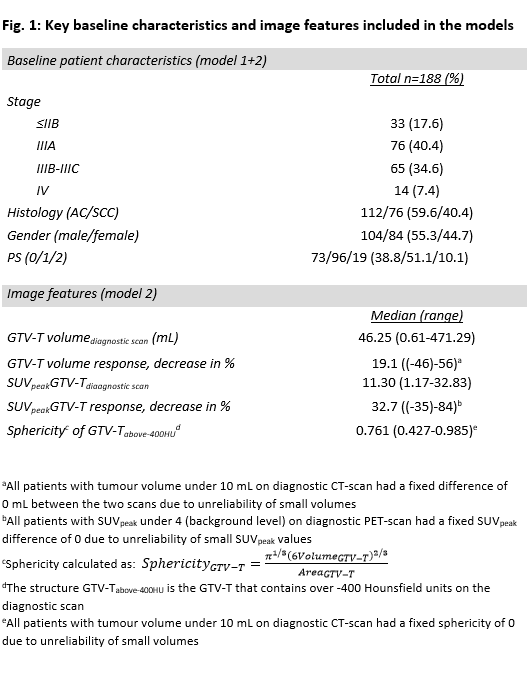
Patients with LA-NSCLC treated with curative
intended cRT (2012-2019) at a single institution were retrospectively reviewed
(n=188). All patients had diagnostic PET/CT-(dPC) and planning PET/CT (pPC)-scans,
between which they received platinum-based chemotherapy. Volume, sphericity and
SUVpeak for the gross tumour volume (GTV-T) were investigated on dPC
and pPC. First failure was characterized as either loco-regional (LR), distant
metastasis (M), simultaneous (LR+M) or death with no evidence of disease. Two multivariate
competing risk analyses (Fine-Gray model) were performed, including patient
characteristics only (Model 1) and patient characteristics, baseline and
changes of image features (Model 2). The variables
included are given in Fig. 1. The models are described with sub-distribution
hazard ratios (SHR) with 95%-Confidence intervals for each failure mode. Cumulative incidences were plotted
for discrete subgroups with the strongest effects in multivariable modelling and
a Fine and Gray test was
used to test for difference in each of the outcomes.
Results
Median follow-up for patients alive was 33
months. Baseline image features on dPC as well as changes between dPC and pPC in
response to chemotherapy varied greatly. Median decrease in GTV-T volume and
SUVpeak were 19.1% and 32.7%, respectively (fig. 1). In Model 1,
histology was the only significant prognostic factor. Squamous cell carcinomas
(SCC) presented a significantly lower risk of M failure (SHR=0.246 [0.0887-0.684],
p<0.01), and higher
risk of LR failure (SHR=2.15 [1.09-4.21], p=0.026) compared to adenocarcinomas (AC). In Model 2, SUVpeak at
diagnosis was the only significant predictor of LR failure (SHR=1.07 [1.02-1.13], p<0.01), while
histology was still the significant predictor of M failure (SHR=0.259 [0.0970-0.694],
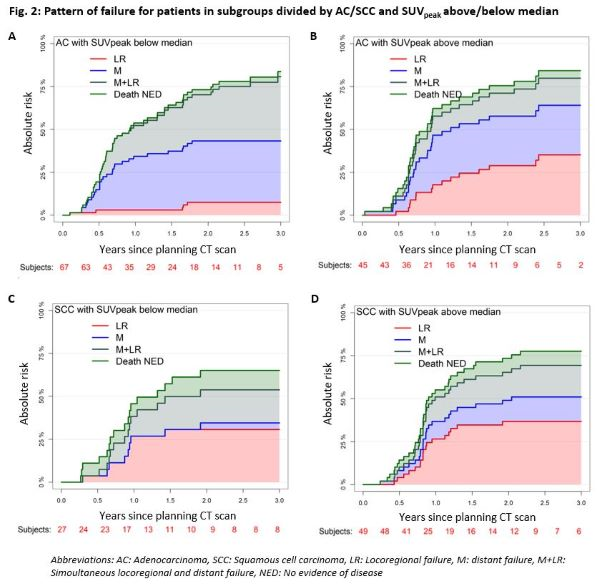
p<0.01, SCC). Analysis on four subgroups (histology, SUVpeak
above and below median) by Fine and Gray tests showed significant difference for LR (p<0.01), M
(p<0.01) and LR+M failure (p=0.048) between the four groups. Cumulative
incidence plots for the four subgroups (fig. 2) illustrate that the incidence
of M failure varies with histology, but not with SUVpeak. For LR
failure, ACs with high SUVpeak are notably more prone to failure than
ACs with low SUVpeak. For SCC, the incidence of LR failure is
independent of SUVpeak.
Conclusion
Histology and tumour SUVpeak at
diagnosis were significant predictors of LR failure in a multivariate model
based on 188 LA-NSCLC patients treated with cRT. AC patients with high SUVpeak
had a higher risk of LR failure than those with low SUVpeak, while
the risk of M failure depended solely on histology.