Treatment patterns and prognosis in inoperable stage III NSCLC treated with concurrent CRT +/- ICI
Benedikt Flörsch,
Germany
PO-1252
Abstract
Treatment patterns and prognosis in inoperable stage III NSCLC treated with concurrent CRT +/- ICI
Authors: Benedikt Flörsch1, Julian Taugner1, Lukas Käsmann1, Saskia Kenndoff1, Julian Guggenberger1, Amanda Tufman2, Niels Reinmuth3, Thomas Duell3, Claus Belka1, Chukwuka Eze1, Farkhad Manapov1
1University Hospital, LMU Munich, Department of Radiotherapy and Radiation Oncology, Munich, Germany; 2University Hospital, LMU Munich, Department of Internal Medicine V, Munich, Germany; 3Asklepios Lung Clinic, Department of Oncology, Munich-Gauting, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate the impact of treatment
developments on outcome in patients with inoperable stage III non-small cell
lung cancer (NSCLC) treated with concurrent chemoradiotherapy (cCRT) +/- immune
checkpoint inhibition (ICI) between 2011 and 2020.
Material and Methods
All consecutive patients treated in a single tertiary
cancer centre were included. Patients were stratified by treatment year and
divided into three subgroups: 2011–2014, 2015–2017 and 2018–2020. Patient- and
treatment-related characteristics, including use of ICI, radiation technique,
PTV>700cc and total lung V20 of more than 30% (V20MED30) were analysed. Planning target volume (PTV) included primary tumor,
involved nodes and safety margins. The primary endpoints were progression-free
(PFS) and overall-survival (OS). All survival parameters were calculated from
the last day of cCRT.
Results
In total, 136 consecutive patients were
included. Median follow-up (FU) was 35.7 (range: 0.9–111.9) months; median age
was 66.9 (range: 48.9–82.5) years; 93 (68%) were male. Fifty-six (41%) patients
had squamous-cell-carcinomas and 69 (51%) adenocarcinomas. All patients
completed conventionally fractionated cCRT to a total dose ≥ 60.0 Gy; 82 (60%) received
VMAT, while 35 (26%) received three-dimensional conformal radiotherapy (3D-CRT).
Median PTV was 700 cc (range: 172.5–2293.2). Thirty-six (26%) patients received
additional ICI with either durvalumab or nivolumab.
The median PFS in the 2011-2014, 2015-2017
and 2018-2020 subgroups was 8.0 (range: 0.7 – 111.9), 8.2 (range: 0.4 – 55.0)
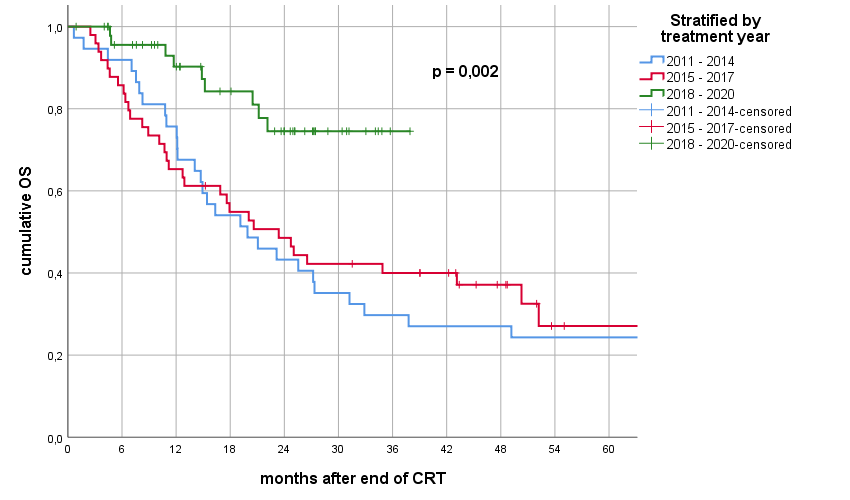
and 26.3 (range: 0.9 – 37.9) months, respectively (p = 0.006). The median OS
for patients treated from 2011-2014 and 2015-2017 was 19.9 (range 0.7 – 111.9) and
23.4 (range: 2.5 – 69.4) months, while it was not reached for patients treated between
2018 and 2020.
In the univariate analysis, ICI
application was a significant prognosticator for PFS (p = 0.002) and OS (p = 0.001).
Similarly, radiotherapy in VMAT technique was associated with significantly
improved PFS (p = 0.001) and OS (p = 0.001), while PTV>700cc (p = 0.011) and
V20MED30 (p = 0.030) were also significant prognosticators for shorter PFS and PTV>700cc
(p = 0.001), ≥20 pack-years (p = 0.029) and V20MED30 (p = 0.002) were
significantly associated with worse OS. In the multivariate analysis, only PTV>700cc
remained a significant prognosticator of PFS (p = 0.038). However, a clear trend
for ICI was observed (p = 0.059). Furthermore, PTV>700cc (p = 0.003),
V20MED30 (p = 0.015), ≥20 pack-years and ICI (p = 0.032) remained significantly
associated with OS.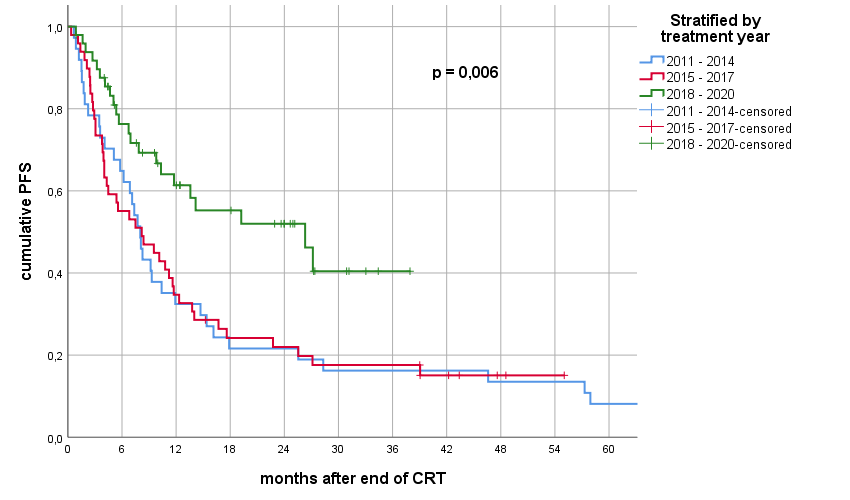
Conclusion
The present analysis demonstrated that in
a cohort of inoperable stage III NSCLC patients treated with cCRT +/- ICI during
the last decade, PTV>700cc, V20MED30, ≥20 pack-years and ICI are important prognosticators
of survival outcome.